Authors:
Sanjeev Tuli, MD
Professor, University of Florida, Gainesville, Florida
Ruchita Kachru, MD
Assistant Professor, University of Florida, Gainesville, Florida
Casey Beal, MD
Assistant Professor, University of Florida, Gainesville, Florida
Sonal Tuli, MD
Professor, University of Florida, Gainesville, Florida
Citation:
Tuli S, Kachru R, Beal C, Tuli S. Episcleritis. Consultant. 2020;60(1):23-24. doi:10.25270/con.2020.01.00005
Disclosure:
This article was supported in part by an unrestricted grant from Research to Prevent Blindness.
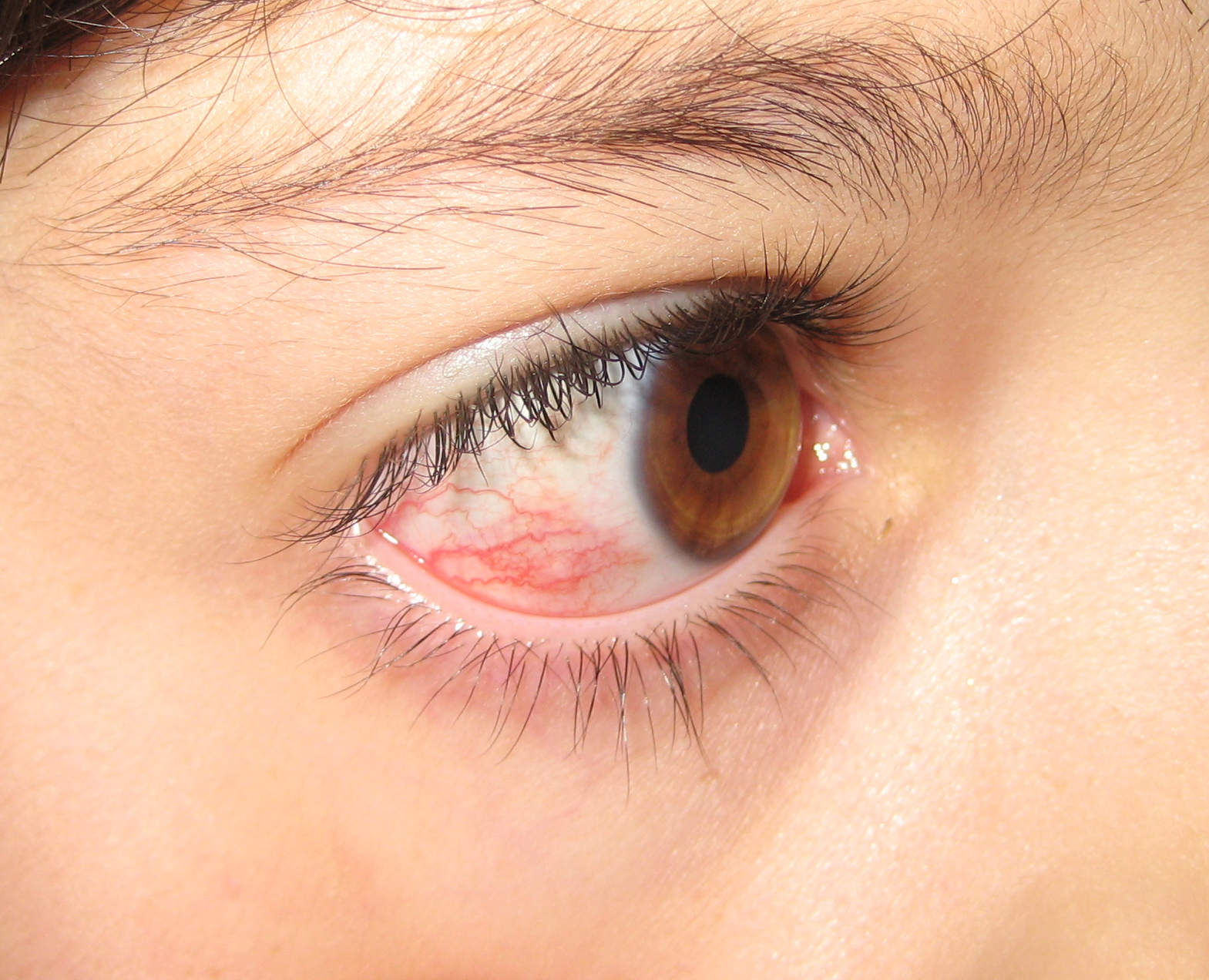
An 8-year-old girl presented with a red area in her right eye (Figure 1). She reported that the lesion had appeared approximately 2 days prior to presentation. She denied any pain, decrease in vision, photophobia, or discharge from the eye. The other eye appeared completely normal. She denied any fevers, joint pain, swollen lymph nodes, and exposure to other children with red eye.
Findings of a review of systems were normal. Her mother reported that the girl may have had a similar episode a few months ago, but it had resolved on its own in 2 to 3 days.
On physical examination, the patient was afebrile, alert, active, and in no apparent distress. Her vital signs were within normal limits for her age. Systemic examination findings were completely within normal limits.
Her visual acuity measured 20/20 in both eyes. The pupils were equal and reactive to light with no evidence of a relative afferent pupillary defect. Ocular motility test results were normal. The eyelids and eyelashes demonstrated mild flaking suggestive of anterior blepharitis (Figure 2).

The conjunctiva showed an area of injection with ill-defined margins in the temporal quadrant. The vessels were tortuous, appeared to be superficial, and could be moved with a cotton-tipped applicator after topical anesthesia instillation. The region was nontender to the touch and blanched with phenylephrine drops, 2.5%. The cornea, anterior chamber, and lens were clear, and the fundus was visualized well. The other eye was completely normal except for mild anterior blepharitis of the eyelids.
Based on the patient’s presentation and physical examination findings, she received a diagnosis of simple episcleritis of the right eye.
DISCUSSION
Episcleritis is an inflammation of the episcleral tissues between the conjunctiva and the sclera. Its cause is unknown, although a very small percentage of cases are associated with autoimmune disorders or are a response to local conditions such as blepharitis or rosacea.
Episcleritis is characterized by injection that is usually localized to a sector of the conjunctiva in the interpalpebral area (the area of the conjunctiva that is exposed when the eye is open). In a minority of cases, the injection may be diffuse over the entire conjunctiva and rarely may be bilateral. The redness is usually asymptomatic, although the patient may report mild, vague discomfort. There is usually no discharge from the eye and no vision complaints. Patients often have a history of multiple similar episodes in the past that resolved spontaneously in a few days.
Episcleritis is of two types, simple and nodular. Simple episcleritis is more likely to be asymptomatic and have no associated underlying condition. Nodular episcleritis, on the other hand, may be associated with mild discomfort, and a small number of cases may be associated with an underlying systemic cause such as rheumatoid arthritis or lupus. The injected area is raised, more well-defined, and may be mildly tender.
The injection in episcleritis is bright red in color with tortuous vessels. This is best visualized in daylight rather than artificial light to distinguish it from the violaceous color of scleritis. The vessels are tortuous and superficial and can be moved over the underlying sclera. Diffuse episcleritis will have ill-defined margins, with the injection gradually fading into the surrounding conjunctiva. The lesion is usually nontender. Instillation of phenylephrine eye drops, 2.5%, will blanch these superficial vessels.
In approximately 10% of cases, small corneal opacities may be present on the peripheral cornea adjacent to the episcleritis. Very elevated nodular episcleritis may be associated with a thinned area (dellen) on the cornea adjacent to it, resulting from a lack of wetting.
DIFFERENTIAL DIAGNOSIS
Conjunctivitis is characterized by injection that is much more diffuse over the conjunctiva. Patients will typically report a foreign-body sensation (infectious) or itching (allergic) and may report that their eyelids are stuck together on waking up. There is usually copious discharge that may be clear (viral), stringy and mucoid (allergic), or mucopurulent (bacterial). The injection is greater in the fornices than around the cornea. There may be preauricular lymphadenopathy with viral conjunctivitis. Viral conjunctivitis is usually bilateral, while bacterial conjunctivitis is usually unilateral.
Scleritis is associated with severe pain that is described by patients as throbbing or a boring sensation. The injection is more violaceous, and the vessels are straighter, larger, and deeper. The injection does not blanch with phenylephrine; the area is immobile and exquisitely tender to the touch. Scleritis is frequently associated with an underlying connective tissue or autoimmune disease. It is exceedingly rare in children.
Phlyctenulosis is a hypersensitivity reaction to eyelid bacteria such as staphylococci and rarely mycobacteria. It is characterized by a nodule on the conjunctiva or cornea with a leash of vessels behind it. The nodule can march across the cornea, causing significant vision problems. The symptoms include severe photophobia, and examination of the eye usually reveals classic triangular scars that are the residua of previous episodes.
MANAGEMENT
Episcleritis is usually a self-limited condition that resolves spontaneously within 1 to 2 weeks without treatment. No residual damage to the ocular tissues and no loss of vision are associated with this condition. Patients with episcleritis typically do not need extensive laboratory evaluations unless they have a history suggestive of an underlying systemic disorder or do not respond to medical management.
Artificial tears for comfort and eyelid hygiene are first-line therapy. The initial treatment typically consists of a mild topical corticosteroid such as fluorometholone ophthalmic, 0.1%, four times daily. Patients usually respond very rapidly to this measure. If this treatment fails to control the episcleritis, more frequent instillation or a more potent corticosteroid such as prednisolone acetate ophthalmic, 1%, is used.
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) such as ketorolac anecdotally have been shown to be beneficial in some cases, but controlled studies have not shown a benefit compared with placebo. Oral NSAIDs, usually indomethacin, can be used in recalcitrant cases. These patients are more likely to have an underlying immunologic condition and need a systemic workup. This usually includes serology tests for rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, and polyarthritis nodosa, and workups for tuberculosis and syphilis.
PATIENT COURSE
The patient’s parents were reassured that this was a self-limited condition. The girl was prescribed artificial tears 4 times a day, and the parents were instructed to use warm compresses and eyelid scrubs to eliminate the blepharitis. She returned after 2 weeks with complete resolution of her symptoms. Her parents were informed that the condition could recur and about the importance of eyelid hygiene.
REFERENCES:
- Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol. 2000;130(4):469-476.
- Yanoff M, Cameron D. Diseases of the visual system. In: Goldman L, Schafer I, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2011:2426-244


