Peer Reviewed
Entropion: Etiology, Classification, Diagnosis, and Treatment
Authors:
Leonid Skorin Jr, DO, OD, MS
Ophthalmologist, Mayo Clinic Health System, Albert Lea, Minnesota
Stephanie Norberg, OD
Resident optometrist, Minneapolis VA Medical Center, Minneapolis, Minnesota
Jacob A. Erickson, OD
Optometrist, Shopko Eyecare Center, Albert Lea, Minnesota
Citation:
Skorin L Jr, Norberg S, Erickson JA. Entropion: etiology, classification, diagnosis, and treatment. Consultant. 2018;58(12):325-335.
ABSTRACT: Ocular foreign-body sensation and conjunctival injection are two very common patient presentations. One possible cause of these symptoms is entropion, or an inward turning of the eyelid margin. Entropion can have an involutional, spastic, cicatricial, or congenital cause. It can be medically managed in the short term, but for full resolution, surgery is typically required. This article reviews the causes, diagnosis, and treatment of entropion. A case report of a 77-year-old man with entropion also is presented.
KEYWORDS: Entropion, eyelid, trichiasis, botulinum toxin
An entropion of the eyelid is characterized by the eyelid margin turning inward.1 Entropion is most commonly due to laxity of the eyelid and often is found in patients older than 60 years.2 Involutional entropion is found in 2.1% of the elderly population.2 This condition has the potential to be painful and visually debilitating to the patient.3
In order to better understand entropion, it is helpful to first take a close look at the anatomy of the eyelids.
Eyelid Anatomy and Physiology
The eyelids play a crucial role in protecting and maintaining hydration of the ocular surface.4 The eyelids are divided into 2 primary parts: the anterior lamella and the posterior lamella. The anterior lamella consists of the skin, eyelashes, glands, and the orbicularis oculi muscle. The posterior lamella consists of the tarsal plate, conjunctiva, and retractor muscles.5 The orbicularis oculi muscle and the posterior lamella are especially important in the development of entropion.
The orbicularis oculi muscle is a large striated muscle that encircles the eye, present just below the skin of both the upper and lower eyelids.6 Its primary role is to firmly close the eye, and it plays a role in spontaneous and reflex blinking. It is innervated by the facial nerve (cranial nerve VII).4 The orbicularis oculi muscle is important in this discussion, because the preseptal portion of the muscle can overact in older patients. When this happens, the inferior portion of the lower tarsal plate gets pulled forward relative to the rest of the tarsal plate, rolling the eyelashes toward the globe.7
Along the lid margin is also located the Riolan muscle. This muscle is considered part of the orbicularis oculi, but instead of closing the eye, it serves to keep a firm apposition of the lid against the globe, acting as one of the retractor muscles of the eyelid.6 After surgery to the eye or the surrounding structures, especially when eyelid edema is present, the Riolan muscle can spasm, leading to the development of spastic entropion.4 This occurrence is especially common when mild involutional changes are already present.
The conjunctiva serves as a covering for both the eyelids and the surface of the globe around the cornea. It is a mucous membrane that is made of 2 main parts: the bulbar conjunctiva and the palpebral conjunctiva, which are joined at the fornix. The bulbar conjunctiva covers the sclera and episclera, while the palpebral conjunctiva covers the inner side of the eyelids.6 Scarring of the palpebral conjunctiva will lead to contraction of the tissue, causing the eyelid margin itself to roll inward. This would cause a cicatricial entropion.8
NEXT: Classification of Entropion
Classification of Entropion
Entropion is grouped into 4 main categories: involutional, spastic, cicatricial, and congenital (Table 1).3

Involutional entropion occurs as a result of age-related changes to the eyelids. There is typically no underlying pathology in this type of entropion. The main cause is laxity of the lower eyelid horizontally. In addition, it can include vertical eyelid instability due to weakness of the retractor muscles of the lower eyelid. Also, with closure of the eyelid, the orbicularis muscle can start to pull the lower edge of the tarsal plate anteriorly, turning the lid margin in toward the globe. This is called overriding of the pretarsal orbicularis. Finally, involutional entropion can be caused by laxity of the orbital septum, which allows prolapse of orbital fat into the lower lid.7
Spastic entropion is closely related to involutional entropion, because it primarily occurs in patients with early involutional changes to the eyelid. The actual entropion is caused by irritation or inflammation of the eyelid in these patients, most frequently after surgery to the eyes or eyelids, particularly surgery that results in eyelid edema.9
Cicatricial entropion occurs when scarring of the eyelid causes shrinkage of the posterior lamella, often occurring secondary to disease.8 The most common cause of these changes is trachoma, which is also a leading cause of blindness worldwide.5 Other possible causes of cicatricial entropion include ocular cicatricial pemphigoid, Stevens-Johnson syndrome, chemical burns, trauma, sarcoidosis, chronic irritation of the eyelids, herpes zoster ophthalmicus, and neoplasm.3,9
Congenital entropion is a very rare condition. Fewer than 50 cases have been reported in the medical literature.8 It can be caused by a number of factors, including defects in the tarsal plate structure, shortened posterior lamella, or an eyelid retractor dysgenesis. An even rarer form of congenital entropion exists, affecting the upper eyelid, called horizontal tarsal kink, in which the upper tarsal plate does not form correctly, resulting in the eyelid margin being bent in toward the cornea.9
Common Entropion Symptoms
When the eyelid is rotated inward such that the eyelid margin, eyelashes, and skin of the eyelids rub against the globe, the result is irritation.5 Most patients with entropion experience generalized ocular irritation, foreign-body sensation, tearing, and a constant red eye.9,10 Other common symptoms of entropion include a burning sensation, photophobia, and blurred vision.5 The eye may look slightly inflamed due to the inturned eyelid margin.5,11 Inversion of the eyelid margin can lead to corneal opacification and severe vision loss.11
NEXT: Diagnosis
Diagnosis
The entropion diagnosis is made by way of an eye examination through an external and biomicroscopy evaluation.10 The eyelid malposition is often visible when the eyelid margin is chronically turned inward, although intermittent entropion cases may appear as if the eyelid is in its normal position adjacent to the globe.5 An inverted eyelid margin can be detected through a few different physical testing techniques, including the orbicularis override test, the snap-back test, the eyelid distraction test, and the digital eversion test (Table 2).

To perform the orbicularis override test, have the patient squeeze his or her eyes shut; a positive finding is a superior migration of the preseptal orbicularis, which will elicit an internal rotation of the eyelid margin (Figure 1).5,10

The snap-back test will show horizontal eyelid laxity in patients with an entropion.11 During the snap-back test, the examiner pulls the lower eyelid downward and releases the eyelid while the patient inhibits blinking.11 The eyelid will return to its anatomical position against the globe within 1 to 2 seconds of release if no pathological laxity is present.10 However, if the eyelid remains below its proper position and away from the globe, pathological laxity is present.10,11
Another simple technique to evaluate eyelid laxity is the distraction test.11 To perform the distraction test, grasp the lower eyelid to pull it anteriorly away from the globe, and measure the distance between the lower eyelid margin and the globe (Figure 2).10,11 Normally, the eyelid margin is withdrawn 2 to 3 mm from the globe, although in cases of eyelid laxity, the distance may be 10 mm or greater.10,11

To differentiate involutional and cicatricial entropion, the digital eversion test may be performed.5 The digital eversion test begins with the examiner pulling the eyelid downward and asking the patient to avoid blinking. If the eyelid margin remains inverted, it is a cicatricial entropion due to shrinkage or retraction of the posterior lamella.5 If the entropion is involutional, then the digital eversion test will obtain a vertical orientation of the eyelid margin.5
When evaluating a patient for entropion, there are several other important differential diagnoses to consider. These are epiblepharon, trichiasis, distichiasis, and ectropion.
Epiblepharon is another condition in which the eyelashes are redirected toward the globe.6 Patients with epiblepharon have an extra horizontal fold of skin along the eyelid margin of the lower eyelid. This extra skin fold causes the eyelashes, which are normally positioned in the lid, to point straight up, so that if the patient looks downward, the eyelashes may contact the cornea. Epiblepharon can look very similar to entropion, and the patient’s symptoms also can be the same. However, if the extra skin on the eyelid margin is pulled downward, the eyelashes will assume a normal position. This is because there is not an actual misalignment of the eyelid, differentiating epiblepharon from a true entropion.7
Trichiasis refers to misdirected eyelashes. In this condition, one or more eyelashes grow out of the follicles directed posteriorly toward the eye.12 This is an acquired condition, and these misdirected lashes can make contact with the corneal or conjunctival surface (Figure 3). If this occurs, the patient can experience the same symptoms of pain, foreign-body sensation, photophobia, and redness that can accompany entropion.4

Distichiasis refers to the growth of a secondary row of eyelashes out of the meibomian glands. Typically, these lashes are much smaller than normal eyelashes, so their presence usually is asymptomatic.12
Ectropion is a result of the eyelid margin turning outward.2,4 Ectropion can cause epiphora, along with exacerbating (or causing) problems with dryness and redness of the conjunctiva.7
NEXT: Treatment
Treatment
Correction of a persistent entropion is essential for maintaining corneal integrity and preventing vision loss. Most entropion cases are managed surgically for a permanent repair of the eyelid margin.1 Nonsurgical medical treatments are an option either while the patient awaits surgical repair or for patients who are poor candidates for surgery.1
To avoid symptoms of irritation, immediate relief can be achieved with the use of topical lubricating ointments and bandage contact lenses to help create a barrier between the ocular surface and the entropic eyelid margin rubbing against the eye.1,5 Entropion can be managed temporarily by taping the eyelid margin so that the eyelashes no longer contact the globe or by epilating the inturned eyelashes with forceps.1,10
Another temporary entropion treatment is botulinum toxin injections.5 The injections block the release of acetylcholine at the neuromuscular junction, causing muscle weakness.13 These injections provide relief for approximately 3 to 4 months by weakening the protractors of the eyelid.5,10 The injections typically start to take effect after 24 to 48 hours, with maximum effect after 1 week.13 The entropion will return after the botulinum toxin injections wear off; thus, repeated injections are required for long-term relief if the patient does not undergo surgery.13
Surgery can offer long-term correction.5 Surgical treatment for an entropion has a success rate of 50% to 80%.13 Entropion is typically treated by reattaching the inferior eyelid retractor muscles to the tarsal plate.1,10 This is followed up by using the lateral canthal strengthening procedure to treat associated horizontal lid laxity (Figure 4).1,10 (View the accompanying Video to watch Leonid Skorin Jr, DO, OD, MS, surgically repair an entropion of the lower eyelid).

Case Report
A 77-year-old man presented with concern for a watery, red right eye. The patient reported rubbing his eyes very frequently and was experiencing a scratchy foreign-body sensation in his right eye.
He mentioned that a physician whom he had seen previously had recommended that he use tape to hold his lower right eyelid away from his eye. The patient discontinued the use of the tape due to irritation of the skin. His visual acuities were 20/60 in the right eye and 20/40 in the left eye. The patient only wore glasses for near work.
The patient received a diagnosis of blepharospasm and involutional entropion of the right lower eyelid (Figure 5). At this visit, he was given a total of 10 units of botulinum toxin injection into the lower eyelid: 5 units laterally, 2.5 units centrally, and 2.5 units nasally. The patient was scheduled for surgical treatment of the entropion, which was successfully completed 6 weeks later.

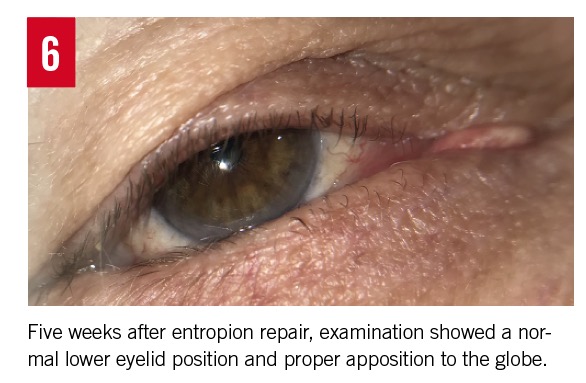
One week postoperatively, it was noted that the patient was healing well, with minimal residual ecchymosis and edema, and the eyelid was now in the correct orientation. At 5 weeks postoperatively, the lid was still in the correct orientation, and the swelling had resolved (Figure 6).
NEXT: Primary Care Considerations
Primary Care Considerations
Entropion is an important condition to be able to recognize and manage, since it can significantly impact patients’ lives. Not only can it potentially cause significant, permanent vision loss, but also it can cause ocular irritation including foreign-body sensation and tearing, thus decreasing the patient’s quality of life.14 This can affect a patient’s physical and psychological well-being.
Entropion is not difficult to diagnose. All of the diagnostic tests discussed here do not require any special equipment or training. Although nonsurgical methods can be used in the short term, treatment of entropion ultimately requires surgery. Once the surgery has been completed, outcomes are typically good. In fact, patient surveys administered after healing from the surgery show a significant improvement in patients’ health-related quality of life.15
Summary
Entropion, or the inward turning of the eyelid margin, can cause foreign-body sensation, tearing, pain, photophobia, redness, and even corneal scarring leading to permanent vision loss. To manage the condition, it is important to differentiate among the different types of entropion. The condition can be managed in the short term with a bandage soft contact lens, epilation of eyelashes, or botulinum toxin injection. Ultimately, surgery is required to resolve the condition. Outcomes of the surgery are typically good and can significantly improve the patient’s quality of life.
References:
- Karesh JW. Evaluation and management of entropion. In: Mauriello JA Jr, ed. Unfavorable Results of Eyelid and Lacrimal Surgery: Prevention and Management. Woburn, MA: Butterworth-Heinemann; 2000:243-259.
- Damasceno RW, Osaki MH, Dantas PEC, Belfort R Jr. Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthalmic Plast Reconstr Surg. 2011;27(5):317-320.
- Gerstenblith AT, Rabinowitz MP. Eyelid. In: Gerstenblith AT, Rabinowitz MP, eds. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012:135-152.
- Cahill KV, Doxanas MT. Eyelid abnormalities: ectropion, entropion, trichiasis. In: Tasman W, Jaeger EA, eds. Duane’s Ophthalmology. Vol 5. Philadelphia, PA: Lippincott Williams & Wilkins, 2013; chap 73.
- Kronish JW. Entropion. In: Chen WP, ed. Oculoplastic Surgery: The Essentials. New York, NY: Thieme Medical Publishers; 2001:chap 3.
- Dutton JJ. The eyelids and anterior orbit. In: Dutton JJ. Atlas of Clinical and Surgical Orbital Anatomy. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2011:129-164.
- Bowling B. Eyelids. In: Bowling B. Kanski’s Clinical Ophthalmology: A Systematic Approach. 8th ed. Philadelphia, PA: Elsevier; 2016:chap 1.
- Gigantelli JW. Entropion. In: Yanoff M, Duker JS, eds. Ophthalmology. 4th ed. Philadelphia PA: Elsevier Saunders; 2014:1278-1283.
- Kaiser PK, Friedman NJ, Pineda R II. Lids, lashes, and lacrimal system. In: Kaiser PK, Friedman NJ, Pineda R II. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2014:67-127.
- Skorin L Jr. A review of entropion and its management. Cont Lens Anterior Eye. 2003;26(2):95-100.
- Myint S. Entropion. In: Onofrey BE, Skorin L Jr, Holdeman NR, eds. Ocular Therapeutics Handbook: A Clinical Manual. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2011:598-600.
- Rubin PAD. Eyelids and lacrimal system. In: Pavan-Langston D, ed. Manual of Ocular Diagnosis and Therapy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:52-56.
- Iozzo I, Tengattini V, Antonucci VA. Senile lower lid entropion successfully treated with botulinum toxin A. J Cosmet Dermatol. 2016;15(2):158-161.
- Dhaliwal U, Nagpal G, Bhatia MS. Health-related quality of life in patients with trachoma, trichiasis or entropion. Ophthalmic Epidemiol. 2006;13(1):59-66.
- Smith HB, Jyothi SB, Mahroo OAR, et al. Patient-reported benefit from oculoplastic surgery. Eye (Lond). 2012;26(11):1418-1423.


