Traumatic Hemorrhagic Chemosis
Authors:
Michael L. Sternberg, MD
University of South Alabama Health University Hospital, Mobile, Alabama
Christopher H. Lasecki, MS-IV
University of South Alabama College of Medicine, Mobile, Alabama
Citation: Sternberg ML, Lasecki CH. Traumatic hemorrhagic chemosis. Consultant. 2018;58(12):349.
A 33-year-old man with autism presented for evaluation of right eye trauma that had been induced by the suction of a vacuum cleaner hose 1 day prior. A history of bilateral glaucoma with medical nonadherence and right eye cataract surgery was obtained from the family, who stated that “he is probably already blind in that eye.”
Physical examination. Conscious sedation was required for an ocular examination, which revealed periorbital ecchymosis, a 4-mm irregular fixed pupil, a cloudy cornea, and a circumferential subconjunctival hemorrhage with prolapse (Figure 1).

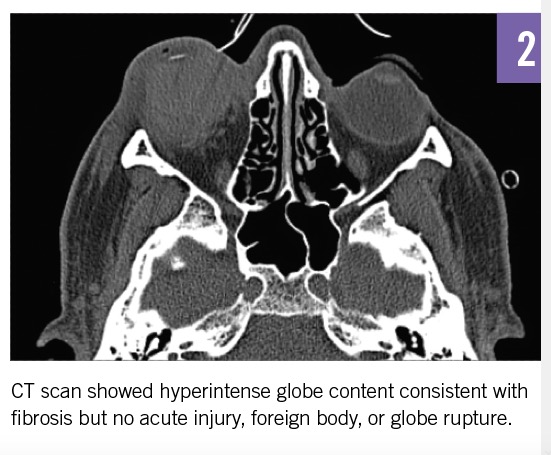
Diagnostic tests. Orbital computed tomography (CT) scan results showed a hyperintense globe content consistent with fibrosis; no acute injury, foreign body, or globe rupture was appreciated (Figure 2). Fluorescein eye stain testing, funduscopic examination, and tonometry revealed a large corneal abrasion, dense intraocular fibrosis, and elevated intraocular pressure bilaterally (right eye, 65 mm Hg; left eye, 55 mm Hg; reference range, 12-22 mm Hg).
Treatment and outcome of the case. A consultant ophthalmologist recommended adherence to a regimen of oral methazolamide and dorzolamide-timolol eye drops to lower intraocular pressure, along with topical erythromycin ointment. The patient achieved baseline status with close follow-up.
Discussion. Traumatic hemorrhagic chemosis from rupture of subconjunctival blood vessels is a frequent result of ocular trauma.1 When the chemosis is circumferential—especially in the setting of an irregularly shaped pupil, hyphema, or shallow anterior chamber—an open globe injury should be suspected. The sclera is thinnest just posterior to the rectus muscle attachments, which themselves are located posterior to the limbus and therefore are the site that is most likely to rupture.2 CT scanning has a specificity of more than 97% but a sensitivity of only 51% to 77% for vitreous hemorrhage and globe contour changes; therefore, early ophthalmologic consultation is essential.3
Gross edema with prolapse may cause prolonged environmental exposure and corneal ulceration and requires aggressive lubrication, shield protection, and occasionally tarsorrhaphy.2 A 2- to 4-week course of treatment is the norm for achieving complete resolution.2
REFERENCES:
- Pargament J, Corrêa ZM, Augsburger JJ. Ophthalmic trauma. In: Riordan-Eva P, Augsburger JJ, eds. Vaughan and Asbury’s General Ophthalmology. 19 ed. New York, NY: McGraw-Hill; 2018:380-389.
- Bord SP, Linden J. Trauma to the globe and orbit. Emerg Med Clin North Am. 2008;26(1):97-123.
- Betts AM, O’Brien WT, Davies BW, Youssef OH. A systematic approach to CT evaluation of orbital trauma. Emerg Radiol. 2014;21(5):511-531.


