A 52-Year-Old With An Abnormal Lesion
History
A 52-year-old male comes in to your office with a 2-view chest x-ray. There is an abnormal finding—an anterior mediastinal lesion. This was discovered during preoperative evaluation for total hip arthroplasty. The patient has a 20-year history of smoking. The patient complains of a mild dry cough, which he has had for several years, and is otherwise asymptomatic.
Laboratory Tests
There are 2 upright radiographs of the chest, a frontal and lateral projection (Figures 1 and 2).

Figure 1. A frontal upright radiograph of the chest demonstrates a mass overlying the right hilum.

Figure 2. A lateral upright radiograph of the chest demonstrates an anterior medistinal lesion.
What do these findings show and do they point to the cause of this patient’s symptoms?
A. Pulmonary embolus/infarct
B. Pneumonia
C. Anterior medistinal mass
D. Pleural effusion
E. Subdiaphragmatic process
(Answer and discussion on next page)
Answer: Thymoma
These conventional radiographs are particularly interesting because they demonstrate several classic principals in radiology. There is an abnormal lesion (3 cm in diameter) on the frontal projection to the right of midline. On the frontal projection (Figure 1), the hilum overlay sign is clearly demonstrated and the right hilum is visualized through the lesion, allowing for localization of the lesion in the anterior or posterior mediastinum. The lesion is not in the middle mediastinum; if it was, it would be causing silhouetting/loss of the detail in the right hilum on the frontal projection.
Additionally, there is elevation of the left hemidiaphragm on the frontal projection. Typically, the left hemidiaphragm is lower than the left. The significance of this is uncertain.

Figure 3. An axial image from CT of the chest confirms the anterior mediastinal lesion.
There is atelectasis at the left lung base. Due to the elevation of the left hemidiaphragm, other factors to consider include adenopathy, an additional small lesion in the region of the aorticopulmonary window, or a lesion in other portions of the mediastinum, which could be causing mass effect upon the phrenic nerve on the left.
The lateral projection (Figure 2) demonstrates that the lesion is within the anterior mediastinum. Unfortunately, the patient was unable to lift his arms well over his head, which made it slightly difficult to appreciate.
The lesion is therefore in the differential diagnosis for anterior mediastinal masses. Classically, anterior mediastinal mass in adults have been described with the pnuemonic the 4 T's: thyroid lesion, a teratoma, terrible lymphoma, and a thymic lesion.
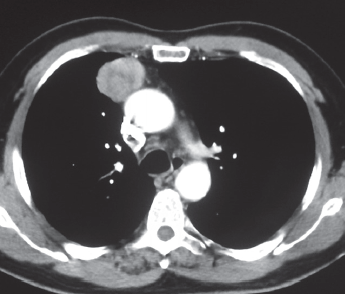
Figure 4. A second axial image from CT of the chest confirms the anterior mediastinal lesion and demonstrates minimal heterogeneity of the lesion.
Other lesions can also be identified in the anterior mediastinum. Always be suspicious of vascular lesions. While these are more typically middle mediastinal lesions associated with the aorta, a sampling of these lesions could lead to disastrous consequences.
Additional Testing
The next logical step is to further investigation with a CT scan of the chest with intravenous contrast. In this particular case, intravenous contrast is helpful as there is a mediastinal lesion. The contrast material aids in identifying different structures within the mediastinum and allows clear visualization of vascular lesions from known vascular lesions due to their enhancement characteristics.
Two consecutive images through the chest showed mediastinal windows (Figures 3 and 4). These demonstrate a lesion in the anterior mediastinum, confirming the findings of the chest radiographs. This lesion is anterior and to the right of the ascending aorta. Close inspection demonstrates the lesion to be just posterior and to the right of the internal mammary artery and vein. The lesion demonstrates minimal heterogeneity. Close inspection also reveals preservation of a fat plane between the lesion and the aorta on the 2 slices visualized by a low-density line.
More cephalad images demonstrate this lesion to be distinctly separate from the thyroid, essentially excluding that the lesion is of thyroidal origin. Importantly, there are no other lesions. The elevation of the left hemidiaphragm remains present. There is no lesion in the aorticopulmonary window.

Figure 5. An axial image from PET CT demonstrates the lesion to have fluorodeoxyglucose avidity (orange) fused to the CT scan for anatomic localization.
The etiology of the elevation of the left hemidiaphragm remains unclear. Given the patient’s history of smoking a lung cancer was suspected, although the absence of other lesions and the location of this particular lesion reduces the likeliness.
The lesion does not contain fat or calcific deposits making a teratoma less likely. Typically, teratomas are in younger patients. Lymphoma is typically in a younger patient population as well. While it cannot be excluded, lymphoma is less likely.
The patient was apprehensive about having a percutaneous biopsy. The clinician then ordered a nuclear medicine positron emission tomography (PET)/CT to confirm that the lesion is metabolically active. There were no old studies available for comparison.
The nuclear medicine PET CT was performed. Axial (Figure 5) and sagittal (Figure 6)images are included. The images presented represent fused data. The nuclear medicine PET portion of the exam is represented in a hot metal scale. The orange in the image represents metabolic activity.
The specific uptake value was >4, which indicates that this lesion is abnormal or a positive scan. Importantly, no other lesions are identified. The nuclear medicine PET scan is typically performed from the skull base to the mid femur. This allows visualization of the entire body to determine if there are extrathoracic sites of disease not visualized with the imaging studies performed thus far.
The patient then agreed to have a percutaneous biopsy, which was performed under CT guidance via an anterior approach. Because the lesion was adjacent to the right lung, care was taken not to cause pneumothorax nor damage the adjacent descending aorta or the smaller internal mammary vessels.
The diagnosis is a benign thymoma.

Figure 6. A sagittal fused image from PET CT demonstrates the lesion to have fluorodeoxyglucose avidity (orange) fused to the CT scan for anatomic localization.
Discussion
Thymoma is the most common anterior mediastinal primary lesion. In some series, it can represent 20% of adult mediastinal masses. Approximately 50% of patients are asymptomatic at the time of presentation. Symptoms are usually related to mechanical compression of adjacent structures, the adjacent lung causing cough, or the adjacent superior vena cava in the aorta causing vascular symptoms.
Thymoma can be associated with myasthenia gravis.
Outcome of the Case
This patient did not have symptoms of myasthenia gravis. This patient was recommended for surgical resection and given an excellent prognosis. n
William Yaakob, MD, is a board-certified radiologist working in Tallahassee, FL.


