Acute Salicylate Toxicity in Children: Diagnosis and Treatment of Overingestion
Abstract: Salicylate and its derivatives are commonly found worldwide in common medications used to treat pain, fever, and inflammation. Despite a decline in popularity, this chemical compound’s ubiquity and accessibility results in it being frequently implicated in childhood drug poisonings. This article reviews the pathophysiology of salicylate metabolism, the clinical and diagnostic clues of an acute overdose, and the cellular response of salicylate poisoning on various organ systems, as well as differential diagnoses and treatment approaches to toxicity in children.
Key words: salicylate, acetylsalicylic acid, aspirin, salicylate poisoning, salicylate toxicity, salicylism, methyl salicylate, ototoxicity, tinnitus, hyperventilation, hyperpnea, respiratory alkalosis, metabolic acidosis, Krebs cycle, oxidative phosphorylation, hyperthermia, seizures, anion gap, sodium bicarbonate, urine alkalinization, Done nomogram
 Salicylate and its derivatives are ubiquitous agents found in over-the-counter and prescription medications. Salicin, a compound first extracted from the bark of willow plant species (Salix), is the precursor of synthetically derived acetylsalicylic acid (ASA), or aspirin. It has served as the primary ingredient in analgesic, antipyretic, and anti-inflammatory medications since the fifth century bc in ancient Greece.
Salicylate and its derivatives are ubiquitous agents found in over-the-counter and prescription medications. Salicin, a compound first extracted from the bark of willow plant species (Salix), is the precursor of synthetically derived acetylsalicylic acid (ASA), or aspirin. It has served as the primary ingredient in analgesic, antipyretic, and anti-inflammatory medications since the fifth century bc in ancient Greece.
Charles Frédéric Gerhardt, a French chemist, synthesized an unstable, impure form of ASA in 1853.1 In 1899, the German pharmaceutical company Friedrich Bayer and Co. patented ASA as a drug under the brand name Aspirin.
The term aspirin originates from a for acetyl; spir for the meadowsweet plant, another botanical source of salicin that had been classified within the genus Spiraea; and the suffix -in, which is commonly used for naming medications.2
Human poisoning from salicylates, also termed salicylism, remains a global concern. Despite the decreased use of ASA-containing medications since the 1960s (as a response to aspirin’s association with Reye syndrome in children), in 2005 the reported number of U.S. ASA and non-ASA salicylate exposures exceeded 20,000 and resulted in 60 fatalities.3
Accidental aspirin overdose has declined over the years as a result of each chewable low-strength aspirin tablet’s ASA dose being limited to 81 mg; low-strength aspirin being limited to 36 tablets per bottle; child-resistant packaging4; and the increased use of medications other than salicylates, such as acetaminophen and ibuprofen, to treat fever, pain, and inflammation in children.5
This review article discusses the pathophysiology of salicylate metabolism, the clinical and diagnostic clues to an acute overdose, the impact of salicylism on cells and organ systems, differential diagnoses, and management approaches for pediatric patients.
The focus of this article is on acute ingestions; however, medical management of chronic toxicity follows the same approach. Chronic salicylism more often occurs in elderly persons, who unknowingly overdose over time on ASA-containing medications taken for cardiovascular protection and/or the daily treatment of painful, chronic conditions such as osteoarthritis.
Salicylate Formulations
Various formulations with different concentrations of salicylates are available, including 81-mg ASA tablets, 325-mg ASA tablets, enteric-coated ASA capsules, and topical methyl salicylate creams and ointments. Familiar brand names of ASA-containing medications are Bufferin, Excedrin, Percodan, Anacin, and Fiorinal.6
Bismuth subsalicylate–containing preparations, such as Pepto-Bismol, are sold over the counter to relieve upset stomach and contain 8.7 mg of salicylate per mL.7
Methyl salicylate, also known as oil of wintergreen, is the most concentrated and toxic formulation of salicylate, containing 98% salicylate in its pure form.
Although it is rare, salicylism from topical salicylate-based applications can occur. Awareness about the differing concentrations of salicylates in topical rubefacients and keratolytics is crucial.5 For example, Greaseless Bengay Pain Relieving Cream contains 15% methyl salicylate, whereas Ultra Strength Bengay Pain Relieving Cream contains 30% methyl salicylate. Body surface area and application frequency are important variables when salicylism from topical agents is suspected.
Pathophysiology
Once ingested, ASA is converted quickly into its active compound, salicylic acid. This moiety is then absorbed in the stomach and the small intestine (primarily the jejunum).8
At therapeutic doses, salicylic acid is metabolized by the liver and eliminated in the urine within 2 to 3 hours after ingestion. Renal sufficiency is critical, since up to 30% of free salicylate can be excreted in urine, with the percentage contingent on urine pH.5 Salicylate urinary excretion is markedly decreased in the presence of renal insufficiency, dehydration, low urine pH (< 6.5), or acidemia.5
 Salicylism affects numerous organ systems, including the neurologic, cardiovascular, pulmonary, hepatic, renal, and hematologic systems. Salicylates affect cellular metabolism in these organ systems by inhibiting Krebs cycle enzymes, uncoupling oxidative phosphorylation, and impeding amino acid synthesis.5 Table 1 outlines the mechanisms of toxic effects in salicylate overdose.
Salicylism affects numerous organ systems, including the neurologic, cardiovascular, pulmonary, hepatic, renal, and hematologic systems. Salicylates affect cellular metabolism in these organ systems by inhibiting Krebs cycle enzymes, uncoupling oxidative phosphorylation, and impeding amino acid synthesis.5 Table 1 outlines the mechanisms of toxic effects in salicylate overdose.
Acid-base status: the anion gap. Understanding the body’s acid-base balance and calculating the anion gap is essential to the proper management of patients with salicylate poisoning. Calculation of the anion gap addresses the difference of commonly measured cations (sodium [Na+] and sometimes potassium [K+]) and anions (chloride [Cl−] and bicarbonate [HCO3−]) in serum. Anion gap is calculated using the following formula:
AG = (Na+) – [(Cl−) + (HCO3−)]
Normal anion gap values range from 10 to 15 mEq/L. In salicylism, the anion gap is elevated, reflecting a higher number of unmeasured anions. Possible etiologies for an elevated anion gap can be recalled using the mnemonic SLUMPED (S, salicylate, seizure; L, lactic acid; U, uremia; M, methanol; P, paraldehyde; E, ethanol, ethylene glycol; D, diabetic ketoacidosis).9
In salicylism, the cellular and tissue processes that contribute to the increased anion gap are numerous and complex; these processes contribute to the body’s state in metabolic acidosis. Early in salicylate poisoning, the respiratory centers are directly stimulated, triggering a primary respiratory alkalosis. Subsequently, mitochondrial dysfunction occurs with the inhibition of the Krebs cycle and an uncoupling of oxidative phosphorylation. Renal insufficiency leads to the accumulation of phosphoric and sulfuric acids. Fatty acid metabolism increases, thereby producing ketone bodies.5
Both (mixed) primary respiratory alkalosis and primary metabolic acidosis can present in patients (especially adults) with acute salicylate poisoning and are strong diagnostic clues. Respiratory alkalosis has been found to be more of a transient phase in children with salicylism. Early development of metabolic acidosis occurs in these cases.10 Patients with mixed acid-base disturbances can have a normal anion gap despite concurrent acidosis; therefore, this value does not exclude salicylate toxicity in this clinical presentation.5
Fluid and electrolyte effects. Compromised hydration status occurs in salicylate poisoning as a result of initial fluid losses from emesis and then insensible losses from hyperpnea and hyperthermia. Patients with severe poisoning are considered to be 10% dehydrated. Dehydration decreases the renal clearance of salicylate. Hypokalemia and hypocalcemia can occur as a result of primary respiratory alkalosis.5
Glucose metabolism. Uncoupling of oxidative phosphorylation increases cellular metabolic activity and may produce clinical signs of hypoglycemia despite normal serum glucose levels. Depletion of intracellular glucose can lead to a mismatch between glucose levels in plasma and cerebrospinal fluid. Consequently, central nervous system (CNS) hypoglycemia (presenting as altered mental status) can occur in the presence of normal-range serum blood glucose levels.5
CNS effects. The degree of CNS toxicity relates directly to the amount of salicylate bound to CNS tissue. Neurotoxicity occurs more often in patients with chronic salicylate poisoning than in those with acute salicylate poisoning. Acidosis worsens CNS toxicity by increasing the amount of salicylate that can cross the blood-brain barrier, thus increasing the CNS tissue levels.
Tinnitus is an initial sign of salicylate neurotoxicity; ototoxicity, with potential hearing loss, is most noticeable when serum salicylate levels reach 20 to 40 mg/dL.10 Other signs and symptoms of neurotoxicity are nausea, vomiting, hyperpnea, and lethargy. Untreated severe salicylism can lead to disorientation, seizures, cerebral edema, hyperthermia, coma, cardiorespiratory depression, and eventually death.5
Respiratory system effects. Salicylate directly stimulates the respiratory center. Six hours postingestion, serum salicylate levels of 35 mg/dL and greater increase the respiratory rate and depth (hyperpnea). Salicylate poisoning can cause noncardiogenic pulmonary edema (NCPE) and acute lung injury. NCPE is a rare complication in the pediatric population and more often is a complication in elderly patients with chronic salicylate toxicity. Severe hypoxia occurs, requiring oxygen delivery and continuous care in a critical care setting. In addition, the presence of pulmonary edema makes it difficult to correct compromised hydration and to treat acidosis with sodium bicarbonate. NCPE is associated with extremely high mortality in children and adults; as such, hemodialysis—considered the treatment of last resort for salicylate removal—is strongly advocated.5
Gastrointestinal (GI) tract effects. Nausea, anorexia, and vomiting are common symptoms related to the toxic effects of salicylism. These symptoms are due to either neurotoxicity or damage to the gastric mucosa. Salicylate disrupts the gastric mucosal barrier and causes GI bleeding. Large doses can further cause pylorospasm and lead to decreased GI tract motility.
Enteric-coated ASA formulations can create concretions and bezoars in the stomach, which act directly as a GI irritant, leading to nausea, vomiting, and abdominal pain.10 In these situations, salicylate elimination is decreased, and the GI tract absorbs an increased amount of salicylate.5 Mild hepatitis can ensue in children with plasma salicylate levels greater than 30 mg/dL as reflected by elevated hepatic transaminase levels.11
Reye syndrome, a salicylate-induced hepatic disease, can occur when ASA medications are taken (especially by children) to alleviate symptoms of a viral infection. This rare condition primarily affects the brain and liver. Characteristic signs and symptoms of Reye syndrome are severe and include persistent vomiting, hypoglycemia, elevated liver enzymes and ammonia, fatty infiltration of the liver, and altered mental status resulting from increased intracranial pressure, eventually leading to coma and death.5
Other systemic effects. Hematologic abnormalities can occur, with the most common being increased bleeding related to hypoprothrombinemia and platelet dysfunction (ie, impaired aggregation). Inhibition of vitamin K–dependent enzymes and formation of thromboxane A2 also may play roles. In addition, the release of heat and energy created by the uncoupling of oxidative phosphorylation can lead to rhabdomyolysis.5
Dosage and Toxicity
Salicylate toxicity can occur in patients of any age. The patient’s age helps clarify the cause of the ingestion. Improper dosing of a patient younger than 1 year of age is termed a therapeutic misadventure, indicating that the infant’s parent or caregiver administered the medication incorrectly. Accidental or unintentional poisonings occur in toddlers and young children who are able to access medications and other toxic substances in an unsupervised environment.
Teenagers and adults may intentionally ingest toxic amounts of aspirin as a means of self-harm. Elderly persons may unintentionally overdose on ASA-containing medications used to treat their chronic illness.
Outpatient medical management also can be a factor. Young children who are diagnosed with Kawasaki disease often are prescribed daily low-dose aspirin as part of their outpatient treatment plan.
For children younger than 12 years old, the recommended weight-based single dose of ASA (oral or rectal) to treat fever or pain is 10 to 15 mg/kg every 4 to 6 hours, not to exceed 4 g per 24-hour period. For patients 12 years of age and older, the dose (oral or rectal) is 325 to 650 mg every 4 hours as needed, not to exceed 4 g per 24-hour period.12
A toxic dose of ASA is 150 mg/kg, and the minimal lethal dose of ASA is 450 mg/kg. The lethal dose of 100% methyl salicylate in children is 4 mL and in adults is 6 mL. A 5-mL dose (1 teaspoon) of methyl salicylate is equivalent to 7,000 mg of salicylate, or 21 full-dose (325 mg) aspirin tablets.13
A clinical tool to quickly determine a patient’s potential morbidity following a single, acute, nonenteric-coated salicylate ingestion is as follows5:
• < 150 mg/kg ingested: no toxicity to mild toxicity
• 150-300 mg/kg ingested: mild to moderate toxicity
• 301-500 mg/kg ingested: serious toxicity
• > 500 mg/kg ingested: potentially lethal toxicity
Salicylate dose and the patient’s age, renal function, and hydration status are all factors in determining the degree of salicylate toxicity. Historically, the severity of risk after a single acute salicylate ingestion has been interpreted using the Done nomogram for salicylate toxicity (Figure).14 Plasma salicylate concentration (y-axis) is plotted based on the time postingestion (x-axis). The x-axis starts at 6 hours postingestion and ends at 60 hours postingestion. A plasma salicylate level greater than 40 mg/dL at 6 hours postingestion indicates mild risk, whereas a level of 90 mg/dL at 6 hours indicates severe risk.
 The Done nomogram no longer is considered to be an accurate tool to predict salicylate toxicity, and its use is now discouraged.10 Instead, salicylate plasma concentration, laboratory test results, and clinical status are relied on to make appropriate treatment decisions and care plans for patients with salicylism.
The Done nomogram no longer is considered to be an accurate tool to predict salicylate toxicity, and its use is now discouraged.10 Instead, salicylate plasma concentration, laboratory test results, and clinical status are relied on to make appropriate treatment decisions and care plans for patients with salicylism.
Clinical Assessment
The classic triad of symptoms in salicylate poisoning is hyperventilation, tinnitus, and GI irritation. Table 2 further outlines the early and late presenting symptoms of acute salicylate poisoning. Clinical changes are defined in 3 phases for untreated patients with a history of acute toxic salicylate ingestion.7 Timely, rapid medical intervention is required to prevent morbidity and mortality.

Phase 1, the early presentation stage (first 12 hours postingestion), is characterized by hyperventilation resulting from salicylate’s direct stimulation of the respiratory center in the brain’s medulla. This diagnostic clue may be mistaken for emotional excitement or anxiety. Concomitant GI symptoms may or may not be present. Vital signs indicate tachycardia and tachypnea. Hyperpnea leads to respiratory alkalosis and compensatory alkalinuria. Potassium and sodium bicarbonate are excreted in the urine. Fever usually is absent in phase 1.5,10
In phase 2, the late presentation stage (12 to 24 hours postingestion), paradoxic aciduria in the presence of respiratory alkalosis occurs when sufficient amounts of potassium and sodium bicarbonate are depleted from the kidneys. Mitochondrial insult becomes clinically evident with changes in vital signs (notably fever) and clinical instability.
Upon initial presentation, patients may receive misdiagnoses of sepsis, myocardial infarction, or agitation associated with psychiatric illness.10
Phase 3 signifies progression toward death (4 to 6 hours postingestion in an infant, or 24 hours or more postingestion in an adolescent or adult). Dehydration, hypokalemia, and worsening metabolic acidosis occur.5 Mitochondrial function becomes significantly impaired. Marked metabolic acidosis leads to pulmonary edema and cerebral edema. Myocardial depression and hypotension occur secondary to acidosis and volume deficits.
Further neurologic compromise develops with seizures secondary to hypoxia, hypoglycemia, and direct neurotoxicity. Cardiopulmonary arrest follows, and then, likely, death occurs.10
Differential Diagnosis
A complete medical history should include present clinical symptoms, past and recent illnesses, past hospitalizations and surgeries, travel history, family history, medication history, recent ingestion history, allergies to medications or foods, and immunization status. This information, in conjunction with a thorough physical examination, can offer diagnostic clues to other possible causes of a patient’s clinical presentation, such as diabetic ketoacidosis, sepsis, iron toxicity, ethylene glycol poisoning, and ethanol poisoning.10
Chronic salicylism can present with a confusing diagnostic picture, delaying an accurate diagnosis. Presenting signs and symptoms may suggest diagnoses such as congestive heart failure, hyperthyroidism, delirium, and psychosis.7
Therapeutic Approach
A patient with a clinical history of toxic salicylate ingestion should be assessed immediately in an emergency department (ED) or other hospital facility. Stabilization of the patient is critical, including completing the ABC (airway, breathing, and circulation) checklist. Possible coingestion of medications such as acetaminophen must be addressed with the patient and/or caregivers, since this information has a direct impact on the medical treatment plan.
In the ED, the patient may be a candidate for oral GI decontamination using activated charcoal. Standard treatment guidelines should be followed, with attention paid to protecting the patient’s airway. Knowledge of the time since ingestion is critical, because successful decontamination with activated charcoal occurs within 2 hours postingestion. An upper limit of 4 hours postingestion also has been cited for decontamination efficacy, especially in the presence of a coingestant that delays gastric motility or when the ingested salicylate is an extended-release preparation.15
Critical initial steps in cases of salicylate overingestion are to place intravenous lines for fluid administration and to obtain blood and urine samples for laboratory evaluation.
Key serum studies are plasma salicylate and acetaminophen levels (if there is a concern about a coingestant), a complete blood count, arterial blood gases, coagulation studies, electrolytes, glucose, calcium, serum ketones, blood urea nitrogen, creatinine, liver transaminases (alanine transaminase and aspartate transaminase), and bilirubin. Complete urinalysis with urine pH is required for additional renal assessment.
Girls and women of childbearing age require a pregnancy test, because salicylate abuse during the first trimester has been associated with pregnancy loss and during the third trimester poses a bleeding risk.
Table 3 summarizes the key points of concern in the management approach to a suspected case of salicylism.
 Treatment
Treatment
The 3-step focus of medical management for salicylism comprises GI decontamination, volume resuscitation, and enhanced elimination. No antidote is available. Medical care should be initiated in the ED and, once the patient has been stabilized, continued in an intensive care setting.
GI decontamination using activated charcoal is the initial step to prevent absorption of salicylate from the stomach and small intestine.15 Activated charcoal decreases absorption and peak salicylate plasma concentrations. The recommended dose is 1 g/kg (maximum 50 g in children and 100 g in adults) with sorbitol. For children, activated charcoal without sorbitol, dosed at 0.5 g/kg, can be given every 4 hours until asymptomatic or plasma salicylate level is less than 40 mg/dL. Gastric lavage is rarely practiced but can be considered as a means of GI decontamination up to 4 hours postingestion if substantial poisoning is suspected (> 500 mg/kg) and the patient has a stabilized airway.10
Volume resuscitation with parenteral fluid should be initiated immediately. Fluid composition to treat metabolic acidosis and to treat salicylism uses 5% dextrose in water with 1 to 2 mEq/kg of sodium bicarbonate added. If hypokalemia is present, 20 to 40 mEq/L of potassium chloride is added to the intravenous fluids. Fluids should be infused intravenously at 1.5 to 2 times the maintenance rate and carefully monitored to prevent fluid overload or pulmonary or cerebral edema. The urine output goal is a minimum of 2 mL/kg/hr.
Elimination enhancement of salicylate occurs with alkalinization of the urine. This process traps salicylate in the renal tubules and increases salicylate excretion. Alkalinization is accomplished by adding sodium bicarbonate to intravenous fluids. Urine pH is maintained above 7.5 (the ideal pH is 8.5) until the patient demonstrates clinical stabilization with improvement in serum electrolyte levels and a plasma salicylate concentration of less than 30 mg/dL.
The ideal goal for arterial blood gas pH is 7.45 to 7.55. A serum pH greater than 7.55 should be avoided to prevent systemic complications associated with metabolic alkalosis.
Laboratory evaluations of blood and urine should be repeated a minimum of every 2 hours until evidence of treatment success is well established.10,16
Hemodialysis to foster salicylate elimination is considered only as a last resort. It is reserved for patients with significant neurotoxicity (eg, focal neurologic signs, seizures, cerebral edema, coma), NCPE, renal insufficiency, a plasma salicylate level greater than 90 mg/dL in acute overdose, intractable acidosis, severe electrolyte disturbances, and/or progressive clinical deterioration.5,7,10
 Inpatient Consultation
Inpatient Consultation
Medical support can be provided by a medical toxicologist, especially for the care of patients in whom there is a concern for coingestion, a complicated past or present medical history, or an atypical clinical presentation.
The knowledge and expertise of medical specialists in critical care, pulmonology, metabolic physiology, and renal physiology are invaluable.
Intentional or unintentional misuse of salicylates requires intervention by the hospital’s social work and mental health teams.
Prognosis
Morbidity and mortality rates vary depending on whether the salicylate poisoning is a result of an acute ingestion or a chronic ingestion. Patients with acute poisoning have a 16% morbidity rate and a 1% mortality rate, whereas morbidity and mortality rates for patients with chronic salicylism are greater, at 30% and 25%, respectively.5
The American Association of Poison Control Centers reports that 24% of analgesic-related deaths are a result of aspirin ingestion alone or ingestion of an aspirin combination medication.3
Early Intervention Is Critical
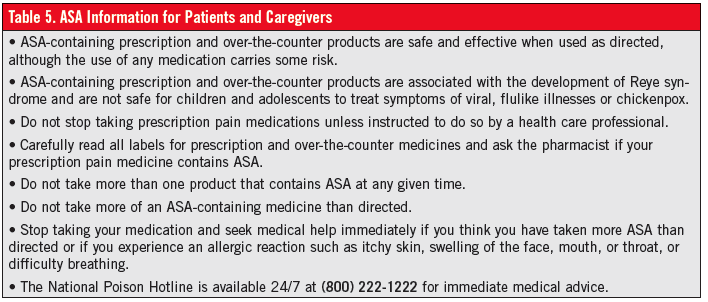
Salicylate poisoning is a serious medical concern, especially among pediatric patients. ASA-containing products are readily accessible, have excellent safety profiles, and effectively relieve pain, fever, and inflammation when administered properly; nevertheless, salicylism remains a leading cause of morbidity and mortality in the United States and worldwide.
Early identification of salicylate toxicity and prompt implementation of appropriate treatment can be lifesaving. Continued awareness and public education about the risks of salicylate poisoning aim to further minimize this hazard and increase this drug’s safety profile.
 References:
References:
1.Gerhardt C. Untersuchungen über die wasserfreien organischen Säuren. Justus Liebigs Ann Chem. 1853;87(1):57-84.
2.Cheng TO. The history of aspirin. Tex Heart Inst J. 2007;34(3):392-393.
3.Herres J, Ryan D, Salzman M. Delayed salicylate toxicity with undetectable initial levels after large-dose aspirin ingestion. Am J Emerg Med. 2009;27(9):1173.e1-1173.e3.
4.Walton WW. An evaluation of the Poison Prevention Packaging Act. Pediatrics. 1982;69(3):
363-370.
5.Waseem M, Aslam M, Gernsheimer JR. Salicylate toxicity. Medscape Reference. http://emedicine.medscape.com/article/1009987-overview. Updated March 5, 2013. Accessed November 13, 2013.
6.Chyka PA, Erdman AR, Christianson G, et al; American Association of Poison Control Centers; Healthcare Systems Bureau, Health Resources and Sevices Administration, Department of Health and Human Services. Salicylate poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila). 2007;45(2):95-131.
7.Carstairs S. Salicylates. CALL US …, the Official Newsletter of the California Poison Control System. 2009;7(4). http://www.calpoison.org/hcp/2009/callusvol7no4.htm. Accessed November 13, 2013.
8.Clissold SP. Aspirin and related derivatives of salicylic acid. Drugs. 1986;32(suppl 4):8-26.
9.Arterial blood gases and acid-base disorders. In: Chaudhry HJ, Grieco AJ, Macklis R, Mendelsohn M, Mudge GH Jr. Fundamentals of Clinical Medicine: an Introductory Manual. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: chap 15.
10.O’Malley GF. Emergency department management of the salicylate-poisoned patient. Emerg Med Clin North Am. 2007;25(2):333-346.
11.Hamdan JA, Manasra K, Ahmed M. Salicylate-induced hepatitis in rheumatic fever. Am J Dis Child. 1985;139(5):453-455.
12.Aspirin dosage. Drugs.com Drug Information Online. http://www.drugs.com/dosage/aspirin.html. Accessed November 13, 2013.
13.Botma M, Colquhoun-Flannery W, Leighton S. Laryngeal oedema caused by accidental ingestion of oil of wintergreen. Int J Pediatr Otorhinolaryngol. 2001;58(3):229-232.
14.Done AK. Salicylate intoxication: significance of measurements of salicylate in blood in cases of acute ingestion. Pediatrics. 1960;26(5):800-807.
15.Notarianni L. A reassessment of the treatment of salicylate poisoning. Drug Saf. 1992;7(4):292-303.
16.Krause DS, Wolf BA, Shaw LM. Acute aspirin overdose: mechanisms of toxicity. Ther Drug Monit. 1992;14(6):441-451.
Dr Defendi is associate clinical professor of pediatrics at Olive View–UCLA Medical Center in Sylmar, California.


