Adjusting Warfarin Doses
We previously met Agatha, 85-year-old female with noted atrial fibrillation. She was started on 5 mg daily of warfarin for stroke prevention and her INR 4 days later measured at 1.4 (goal 2.0-3.0). She was asked to return to clinic 3 days later. Today, 7 days after initiation, her INR is subtherapeutic at 1.8. How do we adjust her dose in order to attain a therapeutic INR and when should the dose adjustment be instituted?
Dosage
Unlike other medications, the dose of warfarin is adjusted based on the total weekly dose (TWD) as opposed to the daily dose. Although a partial effect of dose adjustments with warfarin may appear as early 48 to 72 hours post-dose, the full anticoagulant effect of warfarin takes approximately 7 days to manifest. The 2012 CHEST guidelines1 provide general information about warfarin adjustments, which suggests omitting doses when INR is sufficiently elevated as well as making a “dose adjustment”—but they do not give explicit directions about how much to adjust the dose.
Historically, when sub- or supratherapeutic INRs are addressed, modulations of 10% to 20% of warfarin doses have been suggested. Given that warfarin is as much an art as it is a science, there likely will not be standard recommendations regarding dose adjustments that can be made for all patients in all scenarios—there is simply too much variability in response to warfarin as well as factors that may be contributing to the sub- or supratherapeutic INR. Based upon previous literature-based recommendations, as well as our own experience with warfarin patients, we will suggest general parameters on how to properly make dose adjustments.
Diet
Since the primary mechanism of action by which warfarin produces anticoagulation is inhibition of vitamin K-dependent coagulation factors, consistency of dietary intake of vitamin K is critical for all patients treated with warfarin. Exogenous administration of vitamin K (whether through diet or pharmacological dosage form) will attenuate the effects of warfarin and reduce the INR (or prevent the INR from rising if already at baseline). Similarly, omission of usual intake of vitamin K rich foods from the diet can result in an INR increase.
Every patient taking warfarin should be informed about the importance of maintaining consistency of vitamin K-containing foods (VKCF). This is not to suggest that VKCFs should be categorized as “good” or “bad”—indeed, many of the VKCFs are particularly nutritious (eg, fresh greens and spinach)—but rather that patients must become informed about which foods are prominent sources of vitamin K and the need to be consistent in the number of servings of these foods ingested on a weekly basis.
Unfortunately, some patients are misinformed that they should completely avoid VKCFs upon starting warfarin therapy. This is not the case and should not be recommended. Clinical trial evidence has shown that diets, which are inclusive of VKCFs, are associated with more consistent and stable INR values than diets in which VKCFs are absent.1 Amongst patients with out-of-range INR results in our anticoagulation clinic, fluctuation in VKCF intake is one of the most common etiologies (despite our routine educational process which stresses appropriate dietary vigilance).
Clinicians need not be concerned about patients whose diets habitually include high amounts of VKCFs; warfarin dosing can be up-adjusted to compensate for essentially any amount of dietary VKCF. It may be helpful to review a weekly dietary log to provide a clear delineation of VKCF for the patient, by pointing out which foods and condiments count as a serving and to establish a baseline VKCF for future comparison in circumstances when out-of-range INRs occur.
When the INR is minimally supratherapeutic (or less commonly, subtherapeutic), consideration may be given to modulation of VKCF in an effort to restore an appropriate therapeutic level. For example, if a patient consumes 2 servings per week of greens and the INR is 3.4 (goal 2.0-3.0), 1 or 2 extra servings of greens could be consumed to lower the INR without adjusting the dose of warfarin. However, an important consideration is the patient’s ability to modify their intake of greens; some patients may be on fixed incomes and unable to afford more greens, or have habituated themselves to the same diet for numerous years leading to difficulties in adjusting from their routine. Hence, the clinician needs to weigh the relative value and convenience of modulating VKCF versus modulating warfarin dosing.
Adherence
Adherence errors are very common, and generally fall into 2 categories.
Missed doses is the most common scenario, with a predictable reduction in the INR as a result. To avoid missed doses, we ask every patient to identify some daily activity that happens at a sufficiently consistent time and to time their warfarin administration at the same time.
Within the category of “missed doses” are 2 additional subgroups: those who thought they were cured and those who have a variety of excuses (eg, prescription ran out, lost bottle, out of town). Clinicians have probably already encountered patients who discontinued their hypertension, seizure, or dyslipidemia medication once the target was achieved. Patients should be clearly informed about the necessity to maintain warfarin administration daily without omissions for the duration recommended by guidelines.
Florida statutes provide fortunate powers to pharmacists, who are allowed to provide patients with sufficient amounts of essential medications on a case-by-case basis until they can reasonably be expected to see their healthcare provider again.
Mistaken doses are almost equally commonplace. For instance, when a patient is taking more than 1 warfarin dosage strength within a week’s interval (ie, 5 mg M/W/F, and 7.5 mg T/Thur/Sat/Sun), we commonly encounter patients who have mistakenly taken a 7.5 mg dose on a day when 5 mg was intended, and vice versa.
Noting the specific date the dose was omitted or doubled will also be important. The more distant the dose discrepancy the less likely it is contributing to today’s INR value. Misadministered doses more than 7 days prior are unlikely to be contributing to an INR and therefore can be disregarded for the purposes of INR interpretation. However, patients should consistently be counseled on the importance of adherence.
Research
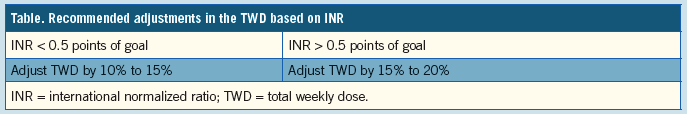
Recent clinical trials evaluating warfarin compared to novel anticoagulants have shed some light on evidence-based approaches to adjusting warfarin therapy. The RE-LY trial, comparing warfarin to dabigatran, created a protocol for adjusting the dose of warfarin based on the INR (Table).2 Since the volume of patients involved in this trial is quite substantial (n=18,000) and since clinical sites following this algorithm had higher time in the therapeutic range (TTR) values compared to sites that did not, we feel it is a sensible protocol to follow when warfarin dose adjustments are required. In order to allow for flexibility in finding an easily obtainable dose using the patient’s current warfarin tablets, in our experience, we adjust by 10% to 15% for INR values <0.5 points and 15% to 20% for INR values >0.5 points from the goal.
Agatha
Agatha reports no change in dietary vitamin K intake (3-4 servings per week, consistent with previous reports), no recent medication changes, and no missed or doubled doses of warfarin. Her INR is subtherapeutic at 1.8 and, as has been said about other scenarios in life, “close only counts in horseshoes and hand grenades.” That is, even a mildly subtherapeutic INR is associated with marked diminution in efficacy of risk reduction for thrombosis. An INR of 1.9 or less is associated with an almost doubling of risk for thrombosis compared to an INR within the therapeutic range. So, a dose increase is likely warranted. Consideration could be given to decreasing intake of greens, but as noted previously, due to the healthful nature of vitamin K-containing foods that would likely be a less prudent step.
Agatha needs a warfarin dose adjustment to bring her INR from 1.8 to at least 2.0 (goal = 2.5, therapeutic range = 2.0-3.0). As her TWD is 35 mg, a 10% to 15% change would lead to an increased TWD of 38.5 mg to 40.25 mg. She has only 5 mg tablets at home, and although there is nothing wrong with providing multiple dosage strengths to fine-tune her warfarin dose, it is more straightforward and simple to adjust dosing based upon the medication she already has.
An increase of 5 mg from her current dose will be an approximate 15% increase (5 mg/35 mg). We prefer to administer and increased dose of warfarin today in order to help the INR begin to increase towards the therapeutic range. If the increased dose is not administered for a few days, then the INR will remain subtherapeutic for longer. Today is Monday, and we know she is subtherapeutic right now and still at-risk of thrombosis, so we should begin the increased dose today. Hence, Agatha was recommended to take 7.5 mg of warfarin on Monday and Thursday, and 5 mg every other day.
Would it be more efficacious to simply administer an extra 5 mg dose today? That is uncertain. What is the optimal interval to administer the new split dose—ie, could it be M/T or M/W? Whether spacing of warfarin doses provides advantage over simply adding to today’s dose has not been studied; hence, our convention has been to divide the dose during the week, hoping to avoid any adverse effects from a peak dose of warfarin, and aim for a smooth transition to the higher dose level. Because the patient takes her warfarin at night, we are able to make this change following today’s clinic visit.
Agatha was counseled to maintain consistent intake of vitamin K, about the importance of adherence, and asked to return to the clinic in 1 week to recheck the INR. Checking sooner than 1 week will likely not allow sufficient time to evaluate the increased dose of warfarin in relation to the INR.
What's the “Take Home”?
1. Evaluating intake of vitamin K-containing foods, drug interactions, and adherence to therapy is necessary when interpreting the INR.
2. Dose adjustments should be made to the TWD of warfarin and in most cases involve a 10% to 20% adjustment in the dose. The dose should be evenly spread throughout the week to minimize differences between the doses and lead to stabilize the INR.
3. Increased or decreased doses should be instituted as early as possible to correct a sub- or supratherapeutic INR, respectively. n
Eric A. Dietrich, MD, graduated from UF College of Pharmacy in 2011 and completed a 2-year fellowship in family medicine where he was in charge of a coumadin clinic. He now works for the UF Colleges of Pharmacy and Medicine.
Louis Kurtizky, MD, is a family physician affiliated with the University of Florida Family Medicine Residency Program, where he commonly co-manages warfarin cases with his colleagues.
References:
1. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: CHEST Evidence-Based Clinical Practice Guidelines. 2012;141(2 Suppl).
2. Van Spall HG, Wallentin L, Yusuf S, et al. Variation in warfarin dose adjustment practice is responsible for differences in the quality of anticoagulation control between centers and countries: an analysis of patients receiving warfarin in the randomized evaluation of long-term anticoagulation therapy (RE-LY) trial. Circulation. 2012;126:2309-2316.


