Peer Reviewed
Mastitis in a Neonate
Authors:
Felicia Fojas, MD, MBS
Elmhurst Hospital Center; Icahn School of Medicine at Mount Sinai, New York
Children’s Hospital of New Jersey at Newark Beth Israel Medical Center, Newark, New Jersey
Maria C. Espiritu-Fuller, MD, MPH
Children’s Hospital of New Jersey at Newark Beth Israel Medical Center, Newark, New Jersey
Meena Kalyanaraman, MD
Children’s Hospital of New Jersey at Newark Beth Israel Medical Center, Newark, New Jersey
Citation:
Fojas F, Espiritu-Fuller MC, Kalyanaraman M. Mastitis in a neonate [published online January 17, 2018]. Consultant for Pediatrians.
A 12-day-old, previously healthy neonate initially had presented to her primary care physician (PCP) after her mother had noticed a small swelling with surrounding erythema near the patient’s left nipple. The swelling had been associated with a small drop of white discharge for 1 day. The PCP had prescribed a course of amoxicillin for a presumed skin infection. However, within a few hours, the erythema and swelling had worsened and was then accompanied by fussiness, vomiting, and decreased oral intake. Therefore, the PCP had advised the mother to have the patient evaluated in an emergency department (ED).
The patient presented to an ED and was subsequently admitted to that hospital’s inpatient pediatric unit.
History. The patient had been born at full term via uncomplicated spontaneous vaginal delivery, with a birth weight of 3.4 kg. There had been no prenatal or postnatal complications. The patient was being exclusively breastfed every 2 hours and had had adequate output. Maternal obstetric history was significant for a group B streptococcal urinary tract infection that had been treated. The mother had been employed as a licensed practical nurse at a nursing home.
Diagnostic tests. At the referring hospital, findings of an ultrasonogram of the left breast were concerning for fluid collection (Figure 1), and the patient was febrile, with a temperature as high as 39.4°C. A full sepsis workup was initiated, and the patient was started on vancomycin and ceftazidime for left breast cellulitis and early abscess.
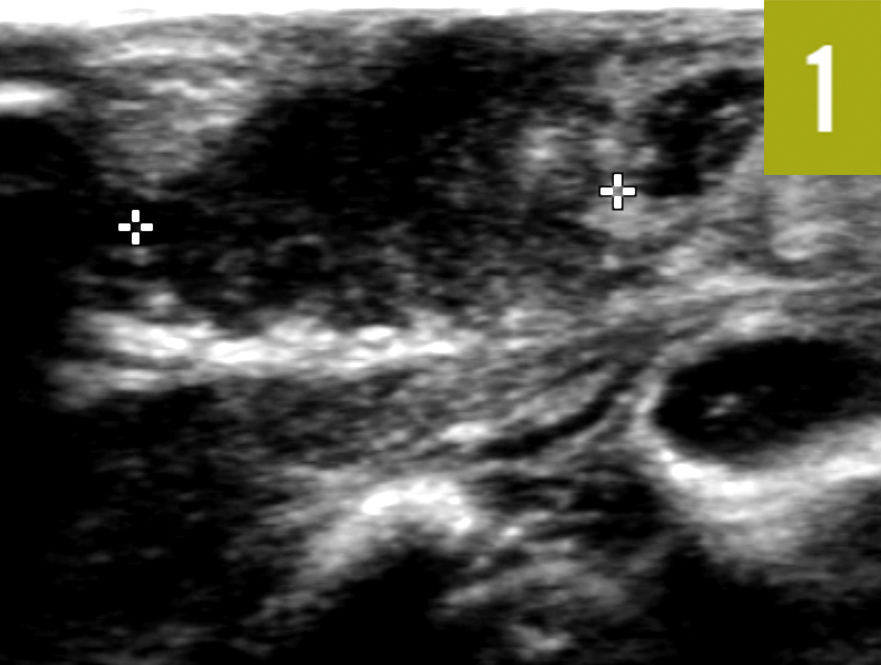
Figure 1. Ultrasonogram of the left breast, taken at the referring hospital, on which heterogeneous hypoechoic fluid collection in subcutaneous soft tissues of the breast can be seen between the calipers.
On hospital day 2, the patient continued to be febrile, with the left breast erythema and swelling spreading rapidly across the chest and to the right flank. A repeated ultrasonogram did not reveal an abscess.
Laboratory test results revealed a white blood cell count of 24,900/µL (reference range, 5000-21,000/µL) with 37% neutrophils (reference range, 34%-68%) and 26% bands (reference range, 5%-11%). The C-reactive protein level was elevated to 34.2 mg/L (reference value, <1.0 mg/L) . The lactate level was 32.4 mg/dL (reference range, 4.5-19.8 mg/dL). Bacterial cultures done as part of the sepsis workup were negative.
Clindamycin was added to the patient’s regimen, and the patient was transferred to our pediatric intensive care unit (PICU) for possible necrotizing fasciitis.
Physical examination. Upon physical examination at our PICU, the patient was afebrile, and vital signs were normal. She was in the 54th percentile for weight and the 55th percentile for length. A nasal swab test result for methicillin-resistant Staphylococcus aureus (MRSA) was negative.
Physical examination findings were significant for an irritable neonate with a 1.5 × 1-cm swelling noted at the left nipple, which was mobile, tender, and nonfluctuant with no drainage. The skin around the swelling was darkly erythematous, raised, and blanching with areas of fluctuance spanning 13 × 7 cm across the chest. Light erythema was noted along the right flank measuring 12.5 × 12 cm and was flat and blanching. All areas of cellulitis were demarcated with a marker (Figure 2).

Figure 2. Physical examination at our PICU showed left-sided mastitis with rapidly progressing cellulitis. Areas of cellulitis were demarcated with a marker.
Vancomycin and clindamycin were continued in the PICU, and tobramycin was added to the regimen. A pediatric surgeon was consulted, whose assessment was that of a complicated chest wall abscess requiring incision and drainage.
Treatment. At the bedside, an incision was made laterally and inferiorly to the left areolar complex. A second incision was made over the sternum. Both areas drained approximately 35 mL of thick, congealed yellow pus. Cultures of the drainage revealed MRSA susceptible to clindamycin and vancomycin. Clindamycin was discontinued, and vancomycin and tobramycin were completed for a 10-day course after drainage.
Outcome of the case. The patient improved within hours of the procedure and did not progress to necrotizing fasciitis. She was discharged home to complete 7 days of oral clindamycin and continued to do well. The mother said the patient had completely recovered 1 month after hospital discharge. Later test results revealed that the mother had had nasal colonization with MRSA.
Discussion. Neonatal mastitis is a rare complication of physiological breast hypertrophy in the newborn period. Transient breast hypertrophy can often develop in the early newborn period, likely due to maternal hormones.1,2 Staphylococcus aureus is the causative organism of neonatal mastitis in more than 75% of cases. Other organisms implicated include group B streptococci and Escherichia coli. Most mastitis cases have been in full-term neonates, with girls more often affected than boys by a 2 to 1 ratio.2 This could be because girls have physiological breast hypertrophy for a longer period. Infections commonly develop within in the first 6 weeks of life, with a peak incidence at 2 to 3 weeks. Neonatal mastitis is not common in preterm infants, because their mammary glands are immature.3
Neonatal mastitis is usually localized infections presenting as unilateral breast swelling with surrounding erythema, induration, tenderness, and possible discharge from the nipple and/or fluctuance.1,2,4-6 Occasionally, a patient may have associated systemic symptoms such as fever or irritability.5 As reported by Walsh and McIntosh,3 only 25% to 40% of patients present with fever. Although the exact mechanism of action of neonatal mastitis is not known, Walsh and McIntosh hypothesized that the organisms normally associated with skin flora travel to the breast tissue through the nipple during the period of physiological neonatal breast hypertrophy.3
Given that our patient had mastitis caused by MRSA in a mother with MRSA colonization, we searched the literature about a possible relationship between the 2 scenarios. One study revealed that infants born to mothers with S aureus colonization during pregnancy are more likely to become colonized with the organism in the early neonatal period.7 Colonization peaked at approximately 2 months of age in these infants. One-third of these cases were due to community-acquired MRSA, particularly the USA300 strain. Although vertical transmission was possible, the majority of mother-infant dyads in the study had a seemingly higher rate of early horizontal transmission.7
In addition to a thorough history and physical examination, other diagnostic tests might include blood work, a full sepsis workup, or ultrasonography of the affected area. However, no specific guidelines exist for the management of neonatal mastitis. Most neonates who have a sepsis workup for mastitis reportedly have negative pan cultures, alluding to rare dissemination of the infection.5,8 Most authors recommend at least a complete blood cell count, blood cultures, and empiric parenteral antibiotics with good S aureus coverage, including MRSA, pending culture sensitivities.1,2,4,5,6,8
A full sepsis workup, including lumbar puncture, should be considered in neonates with systemic symptoms such as fever and irritability, especially if they are less than 60 days of age, as seen in our patient.8 Incision and drainage should be done if mastitis is complicated by abscess formation. Although data on the long-term consequences of mastitis are limited, cases have been reported of asymmetry of affected breast, impaired secretory capacity, and anatomical distortion in adulthood.9
It is imperative that clinicians efficiently recognize and effectively treat neonatal mastitis for successful immediate and long-term outcomes.
References:
- Stricker T, Navratil F, Sennhauser FH. Mastitis in early infancy. Acta Paediatr. 2005;94(2):166-169.
- Faden H. Mastitis in children from birth to 17 years. Pediatr Infect Dis J. 2005;24(12):1113.
- Walsh M, McIntosh K. Neonatal mastitis. Clin Pediatr. 1986;25(8):395-399.
- Stauffer WM, Kamat D. Neonatal mastitis. Pediatr Emerg Care. 2003;19(3):165-166.
- Al Ruwaili N, Scolnik D. Neonatal mastitis: controversies in management. J Clin Neonatol. 2012;1(4):207-210.
- Sloan B, Evans R. Clinical pearls: neonatal breast mass. Acad Emerg Med. 2003;10(3):269-270.
- Jimenez-Truque N, Tedeschi S, Saye EJ, et al. Relationship between maternal and neonatal Staphylococcus aureus colonization. Pediatrics. 2012;129(5):e1252-e1259.
- Montague EC, Hilinski J, Andresen D, Cooley A. Evaluation and treatment of mastitis in infants. Pediatr Infect Dis J. 2013;32(11):1295-1296.
- Panteli C, Arvaniti M, Zavitsanakis A. Long-term consequences of neonatal mastitis. Arch Dis Child. 2012;97(7):673-674.


