Pulmonary Emboli and Deep Vein Thrombosis

The day after a 16-year-old Caucasian boy was evaluated in his orthopedist’s office for intermittent swelling of his left lower leg and thigh of 1 week’s duration and leg pain of 3 days’ duration, he experienced shortness of breath and chest pain. He was referred to the emergency department (ED). He had undergone a bunionectomy 10 weeks earlier. His medical history was otherwise unremarkable.
During the orthopedic evaluation, an ultrasound examination of the left leg had shown a distended left femoral vein containing an echogenic clot and markedly decreased flow, consistent with deep vein thrombosis (A). Baseline prothrombin time and partial thromboplastin time were obtained, oral enoxaparin and warfarin were prescribed, and the patient was instructed to wear compression stockings.
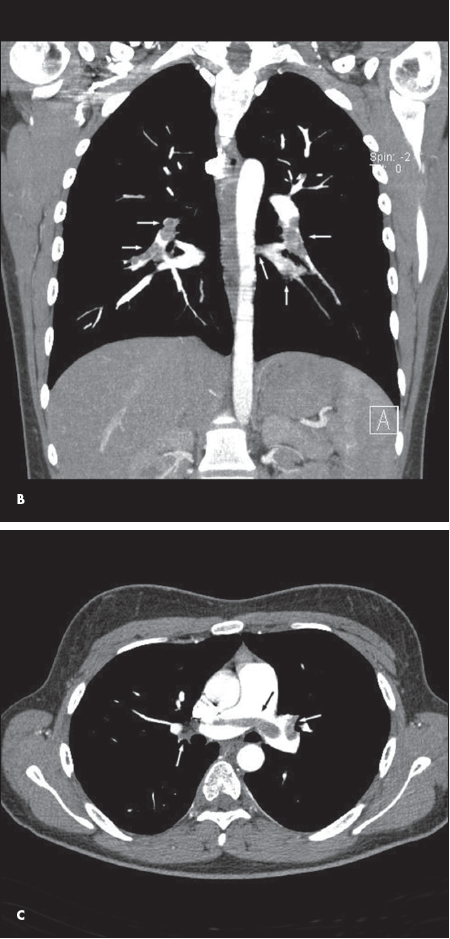
In the ED the next day, a chest CT scan revealed bilateral pulmonary emboli (PE). The coronal view showed bilateral PE in the lobar branches (B, white arrows). The axial view showed bilateral PE in the main pulmonary artery (C, white arrows).
PE and deep vein thrombosis (DVT), although common in adults, are rare in children. However, the conditions are associated with significant morbidity and mortality in both pediatric patients and adults.1 PE may develop with DVT and can present with shortness of breath and/or chest pain.2 A high level of suspicion is essential to make the diagnosis and begin treatment.3 Early recognition and appropriate management of DVT and PE can lead to complete recovery, as was the case in this 16-year-old boy.
Lower and upper extremity DVT is best diagnosed by color Doppler ultrasound imaging, which is readily available, can be done as a portable or bedside examination, and requires no intravenous contrast material or ionizing radiation. The sonographic findings are distention of the involved vein, which is filled with low-level internal echoes representing the clot; lack of color flow on color Doppler interrogation; and loss of the normal augmentation response when the calf is squeezed (see A).
On contrast-enhanced CT scans, PE is characterized by filling defects in the involved pulmonary artery (see B and C). The rapid scanning and improved spatial resolution of multirow helical scanners allow even small emboli in segmental arteries to be identified. CT has replaced nuclear medicine lung scans for the diagnosis of PE in all but a few patients with prior severe contrast reactions or significantly decreased renal function.


