Lymphocytic Hypophysitis
A 26-year-old woman at 30 weeks’ gestation presented to the emergency department with a throbbing frontal headache of 1 month’s duration. She had also had peripheral blurred vision for the past 2 weeks. Acetaminophen initially decreased her pain but was no longer effective. She had had a previous miscarriage.
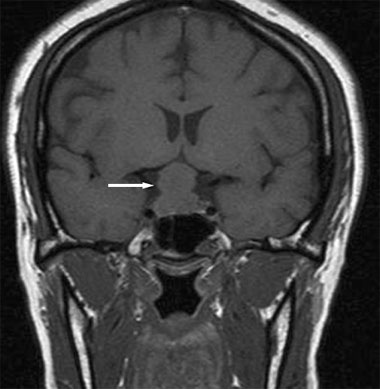
The patient was afebrile. Blood pressure was 120/82 mm Hg. Mild nystagmus was present on horizontal gaze. There were no other pertinent physical findings or abnormal laboratory results. An MRI scan of the head revealed a 2.2-cm suprasellar mass with compression of the optic chiasm (arrow).
A pituitary adenoma was suspected, and the patient underwent transsphenoidal resection of the pituitary gland. Diabetes insipidus developed secondary to the pituitary gland resection. She responded appropriately to a course of desmopressin and was discharged.
Histopathological examination of the pituitary gland revealed lymphocytic hypophysitis, without evidence of pituitary adenoma. Lymphocytic hypophysitis—an autoimmune disorder in which lymphocytes infiltrate and cause destruction of the anterior pituitary gland—is associated with pregnancy and can occur anytime from the late prenatal period until 1 year postpartum. Although the affected pituitary gland initially enlarges, it eventually atrophies and fibrosis develops. Biopsy of the gland reveals lymphocyte and plasma cell infiltration.1 Rarely is a lymphocytic hypophysitis mass found to be larger than 1.5 cm.2
The common presentation is peripartum pituitary failure, vision loss, headache, and hyperprolactinemia. Surgical resection is often unnecessary, because the inflammatory process usually resolves after several months of corticosteroid therapy, with possible restoration of normal pituitary function depending on the amount of tissue destruction.3
1. Bellastella A, Bizzarro A, Coronella C, et al. Lymphocytic hypophysitis: a rare or underestimated disease? Eur J Endocrinol. 2003;149: 363-376.
2. Rivera JA. Lymphocytic hypophysitis: disease spectrum and approach to diagnosis and therapy. Pituitary. 2006;9:35-45.
3. Gutenberg A, Hans V, Puchner MJ, et al. Primary hypophysitis: clinical-pathological correlations. Eur J Endocrinol. 2006;155:101-107.


