AUTHORS:
Mariam Kirvalidze, DO
Family Practice Resident, Peconic Bay Medical Center, Riverhead, New York
Sandeep A. Gandhi, MD
Infectious Diseases Consultant at Peconic Bay Medical Center, Riverhead, New York, and Associate Professor of Clinical Medicine, New York Institute of Technology College of Osteopathic Medicine, Old Westbury, New York
CITATION:
Kirvalidze M, Gandhi SA. Hepatic and pulmonary abscesses from Fusobacterium nucleatum infection. Consultant. 2020;60(2):57-58. doi:10.25270/con.2020.02.00006
An 80-year-old man with a history of type 2 diabetes mellitus, end-stage kidney disease on hemodialysis via a left arteriovenous fistula, and hypertension presented with a dry cough and had had a syncopal episode during a hemodialysis session.
Physical examination revealed a well-developed man with poor dentition. The remainder of the examination findings were unremarkable. Vital signs included a temperature of 37.2°C, a pulse of 76 beats/min, and a blood pressure of 104/50 mm Hg.
His white blood cell count was 20,200/μL with 89% neutrophils. The hemoglobin level was 9.2 g/dL, and the platelet count was 402 × 103/μL. Liver function test results were normal.
Chest radiography showed a new right lower lung mass. A chest computed tomography (CT) scan with contrast revealed a 3.7-cm cavitary lesion in the left upper lobe of the lung and an 8.3-cm necrotic-appearing cavitary lesion in the right lower lobe (Figure 1).

Figure 1. CT scan with contrast showing a right lower lung abscess.
A subsequent CT scan of the chest, abdomen, and pelvis with contrast demonstrated a lung abscess and a 9.0-cm, multilocular, rim-enhancing liver abscess (Figure 2).

Figure 2. CT scan with contrast showing a multilocular, rim-enhancing liver abscess.
Culture of the liver abscess grew Fusobacterium nucleatum, identified by matrix-assisted laser desorption ionization time-of-flight mass spectrometry (Figure 3).
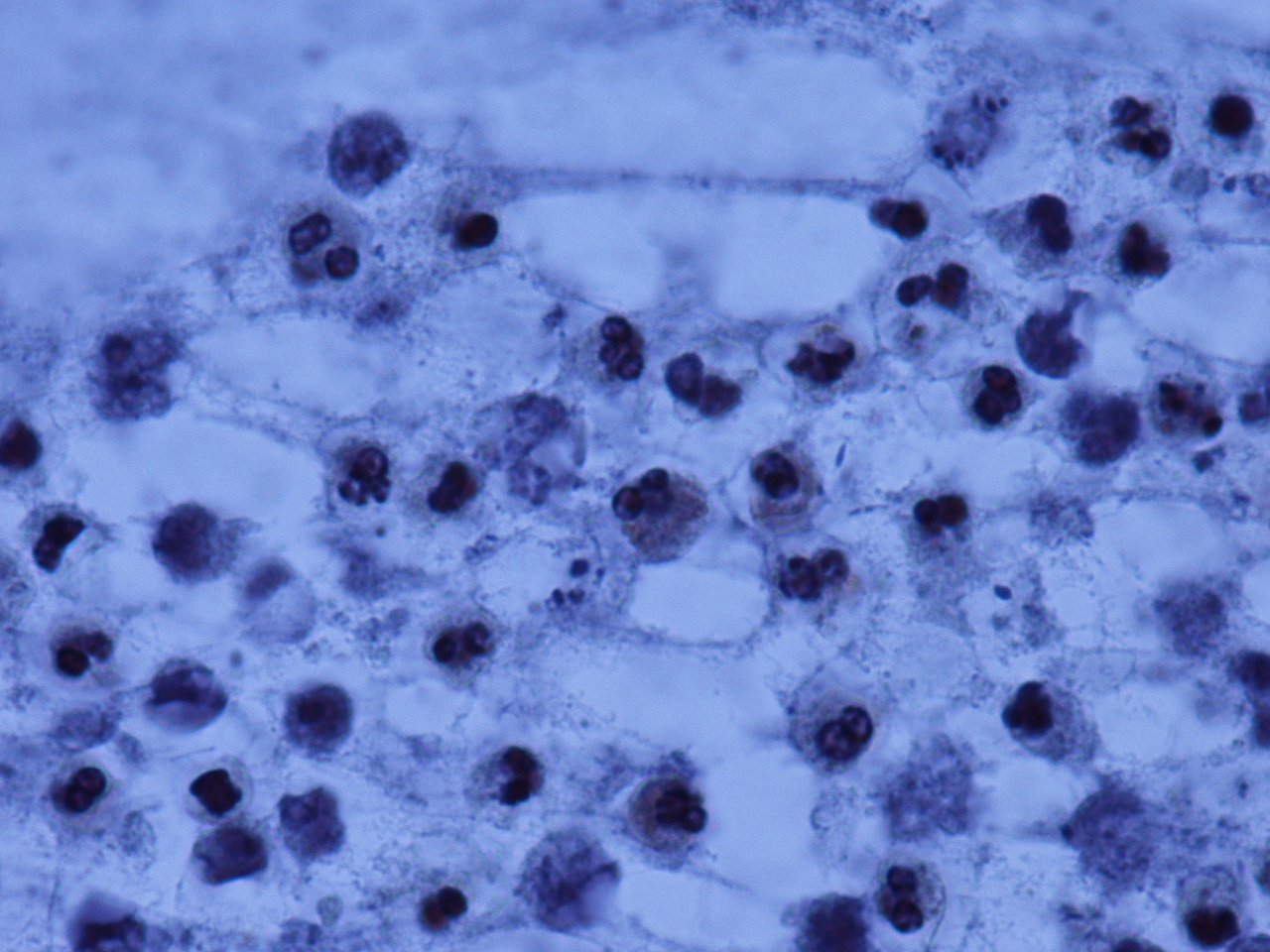
Figure 3. Hematoxylin-eosin stain of the liver abscess material, which grew Fusobacterium nucleatum (photo courtesy of Ranjana Mathur, MD).
The hepatic abscess was drained by an interventional radiologist. The patient was treated with piperacillin-tazobactam and metronidazole until the abscesses had radiographically resolved.
Discussion. Fusobacterium species are gram-negative and non–spore-forming anaerobic bacteria. F nucleatum and Fusobacterium necrophorum are the most commonly isolated bacteria in this group.1 F nucleatum is a prevalent part of the oral flora and is usually found in the oropharynx, while F necrophorum is usually found in the appendix.2
F nucleatum is a rare cause of liver abscess.2,3 It also causes endodontic abscesses.4 Historically, Fusobacterium bacteremia is associated with Lemierre syndrome, first recognized in 1936 by André Lemierre as an oropharyngeal infection causing thrombophlebitis of the internal jugular vein and septic emboli to various organs.5 Recent literature has described a gastrointestinal variant of Lemierre syndrome in which F nucleatum causes septic thrombophlebitis of the portal vein and subsequent portal vein hypertension.6-8
A recent literature review of liver abscesses showed infection with F nucleatum in 22 of 48 reported cases.2 The presumed source was the oral cavity, regardless of the presence of dental disease. Fewer cases were presumed to originate from the lower gastrointestinal tract.2 In another published report, F nucleatum bacteremia was detected in 2 of 4 patients with hematologic malignancies with oral mucositis; in another case, the peritonsillar region and soft palate were edematous.9 Another case report reported a liver abscess in a patient with periodontal disease and dental caries.3 The authors presumed that it was hematogenous spread from the oropharynx via the venous system, then traveling via the hepatic artery and seeding the liver.3
Fusobacterium bacteremia risk factors and outcomes of the infection have been analyzed. F nucleatum bacteremia was found in 61% of 72 cases over 11 years in one review.10 F necrophorum bacteremia was not found in patients younger than 40, and patients’ median age was 53.5 years.10 Other risk factors were malignancy, dialysis, dementia, chronic obstructive lung disease, diabetes, and heart disease. Antibiotic resistance is uncommon among Fusobacterium; no cases showed resistance to metronidazole or clindamycin, and only few had penicillin resistance. Mortality in these patients more likely was a result of associated comorbidities.10
The risk factors in our patient were old age, poor dentition, and hemodialysis. We believe the source of the fusobacterial pulmonary and hepatic abscesses to be the oropharynx. The patient recovered successfully with antibiotic therapy and abscess drainage.
REFERENCES:
- Huggan PJ, Murdoch DR. Fusobacterial infections: clinical spectrum and incidence of invasive disease. J Infect. 2008;57(4):283-289.
- Jayasimhan, D, Wu L, Huggan P. Fusobacterial liver abscess: a case report and review of the literature. BMC Infect Dis. 2017;17(1):440.
- Kajiya T, Uemura T, Kajiya M, et al. Pyogenic liver abscess related to dental disease in an immunocompetent host. Intern Med. 2008;47(7):675-678.
- George N, Flamiatos E, Kawasaki K, et al. Oral microbiota species in acute apical endodontic abscesses. J Oral Microbiol. 2016;8:30989.
- Lemierre A. On certain septicæmias due to anaerobic organisms. Lancet. 1936;227(5874):701-703.
- Zheng L, Giri B. Gastrointestinal variant of Lemierre syndrome: Fusobacterium nucleatum bacteremia-associated hepatic vein thrombosis: a case report and literature review. Am J Ther. 2016;23(3):e933-e93
- Mellor TE, Mitchell N, Logan J. Lemierre’s syndrome variant of the gut. BMJ Case Rep. 2017;201 doi:10.1136/bcr-2017-221567.
- Moore JA, Rambally S. Fusobacterium nucleatum bacteremia presenting with portal vein thrombosis: an abdominal Lemierre syndrome? Am J Med. 2017;130(6):e255-e256.
- Terhes G, Piukovics K, Urbán E, Nagy E. Four cases of bacteraemia caused by Fusobacterium nucleatum in febrile, neutropenic patients. J Med Microbiol. 2011;60(pt 7):1046-104
- Afra K, Laupland K, Leal J, Lloyd T, Gregson D. Incidence, risk factors, and outcomes of Fusobacterium species bacteremia. BMC Infect Dis. 2013;13:264.


