Peer Reviewed
Neonate With Acquired Babesiosis
Introduction. A 27-day-old previously healthy male neonate first presented to the emergency department with 1-day history of fever, irritability, and feeding intolerance.
Patient history. The patient was born at 39 weeks by vaginal delivery to a G1P0 mother with normal prenatal results. He received routine nursery care and was discharged at 2 days of age. The patient and his family live in a tick endemic area, and his mother reported finding a tick on the infant’s left ankle area, engorged with blood a week prior to his fever. The mother believed the source of the tick came from the family’s pet dogs. She monitored the bite site carefully and did not notice any signs of irritation or infection, which was consistent with his physical exam that day. His only physical examination finding in the emergency department was a fever of 38.0 °C. He was admitted for a full sepsis workup and began empiric treatment with intravenous (IV) ampicillin, ceftazidime, and acyclovir.
Diagnostic testing. Laboratory results including cerebrospinal fluid (CSF), urine, and blood cultures were all within normal ranges apart from an elevated C-reactive protein (CRP; 41.1 mg/dl) and trace proteins in the urine (10-20 mg/dl). Respiratory pathogen panel and tick panel (ehrlichiosis/anaplasmosis/babesia nucleic acid testing] both returned negative. Given his reassuring workup, he was discharged 2 days after admission upon fever resolution and 48-hour completion of antimicrobials. At his hospital follow-up examination, his vital signs were stable and there were no pathological findings apart from mild upper respiratory tract congestion at the time of his visit.
Two weeks later, he returned to the emergency department with a 1-day history of fever (38.0 °C), congestion, cough, and clay-colored stools. His physical examination showed a febrile infant with fever (38.2 °C), liver palpable 1 cm below the costal margin, and soft nontender abdomen with normal bowel sounds.
His work up in the emergency department was remarkable for thrombocytopenia (53 K/uL) without leukocytosis (7.5 K/uL), anemia (Hgb 10.0 g/dL), hematocrit test, 30%, transaminitis (aspartate aminotransferase [AST], 890 U/L, alanine transaminase [ALT], 850 U/L), hyperbilirubinemia (total bilirubin [TB], 2.6 mg/dL), an elevated CRP (32 mg/dL), and pro-calcitonin (0.85 ng/dL). The patient underwent a second lumbar puncture, which showed that his CSF was within normal range. His respiratory panel came back positive for rhino enterovirus, and his chest X-ray was consistent with small airway disease.
Treatment and management. The patient was admitted for management of sepsis and began IV empiric antimicrobial treatment including IV ampicillin, ceftriaxone, and acyclovir. Ceftriaxone was included instead of ceftazidime at this time because after neonatal age (28 days), the preferred antibiotic for UTI/sepsis/meningitis is IV ceftriaxone.
During the first 2 days of admission, his oral intake progressively decreased, and he remained constipated. His liver transaminases began to downtrend (AST, 605 U/L, ALT: 733 U/L), while hyperbilirubinemia worsened (TB, 3.7 mg/dL, direct bilirubin, 2.5 mg/dL, indirect bilirubin, 1.2 mg/dl) and alkaline phosphatase became elevated (375 U/L) as was his Gamma glutamyl Transferase (182 U/L).
He became visibly jaundiced, and his spleen and liver were not palpable. Following an abdominal ultrasound, pediatric infectious disease and gastroenterology specialists were consulted and recommended testing for Epstein-Barr virus, herpes simplex virus (HSV), toxoplasmosis, cytomegalovirus (CMV), and alpha antitrypsin levels. Serology was positive for CMV IgM, while his CSF, urine, and blood cultures remained negative. On the third day of admission, he became pale and more jaundiced, prompting a repeat complete blood count (CBC), which showed anemia (Hgb, 7.5 g/dL, HCT, 23.3%), neutropenia (absolute neutrophil count [ANC], 0.7 K/uL), and worsening thrombocytopenia (platelets, 28 K/uL) Pediatric infectious disease specialists were consulted again, and recommended Parvovirus-B19 testing and a transfer to a tertiary center.
The tertiary hospital repeated the CBC the following day, which showed severe anemia, low haptoglobin, continued thrombocytopenia, and elevated ferritin. Hyperbilirubinemia worsened (TB, 4.2 mg/dL, direct fraction, 2.6 mg/dL) and transaminitis continued to downtrend (AST, 295 U/L, ALT 490 U/L). A peripheral smear revealed red blood cells with multiple circular inclusion, highly suggestive for Babesia (Figure 1A-B), which was later confirmed by PCR testing. He was diagnosed with severe babesiosis showing parasite burden in 5% to 6.0% of RBC per high power field (HPF).
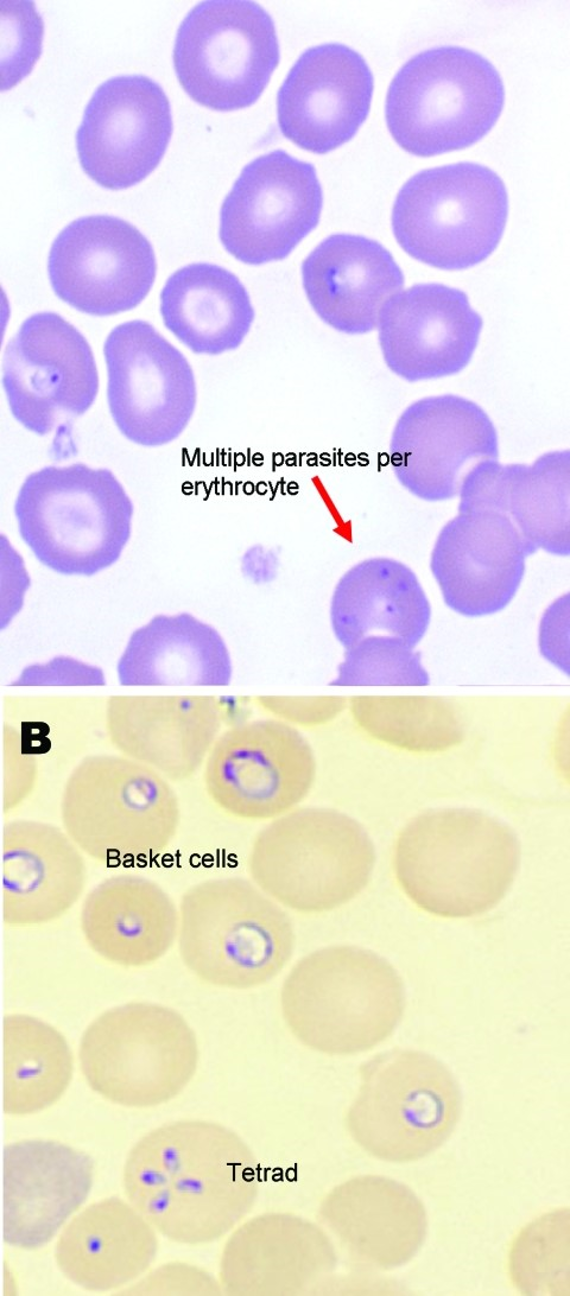
Figures 1A-B. A peripheral smear revealed RBC with multiple circular inclusion, highly suggestive for Babesia, which was later confirmed by PCR testing.
Given his disease severity and rapidly worsening status, pediatric infectious disease and hematology agreed upon dual therapy within exchange transfusion and antimicrobials. The patient tolerated the procedure, showing significant improvement in anemia [Hgb 10.8g/dL, HCT 29.6%] and parasite load, which decreased from 5.0% to 0.5% RBC/HPF on peripheral smear (Table 1).
Table 1. Laboratory data summary
Day of Life | ||||||||||||
Laboratory Data | 1st Hospitalization |
| 2nd Hospitalization | Post Discharge | ||||||||
27 | 47 | 49 | 50 | 50 ¤ | 51 ¶ | 52 | 53 | 54 | 58 | 63 | ||
Lowest Hemoglobin (g/dL)
| 12.4 § | 10.0 | 7.5 | 6.4 | 6.0 | 10.3 | 9.6 | 9.4 | 9.9 | 10.0 | 10.7 | |
Platelet Count (K/uL)
| 176 | 53 | 28 | 28 | 42 | 29 | 39 | 49 | 77 | 325 | 468 | |
Absolute Neutrophil Count (K/uL)
| 3.4 † | 1.0 | 0.7 | 0.3 | 0.6 | 0.3 | 0.4 | 0.3 | 0.4 | 0.5 | 1.1 | |
Total Bilirubin (mg/dL)
| ___ | 2.6 # | 3.7 | 4.2 | 4.2 | 8.2 | 3.6 | ___ | ___ | 0.9 | 0.7 | |
Parasitemia %
| ____ | ____ | ____ | 5.0 | NA | 0.4 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | |
Babesia Present Thick/Thin Smear
| NA | NA | NA | NA |
| NA | Thick Thin | Thick Thin | Thick Thin | Thin | None | |
| *NA, not assessed ¤ Post Platelet and Packed Red Blood Cell Transfusion ¶ Post Exchange Transfusion § Reference Range: 10.0- 16.0 g/dL † Reference Range 1.0-9.0 K/uL # Reference Range: 0.2-1.2 mg/dL | |||||||||||
Differential diagnoses. The differential diagnosis of neonatal babesiosis is broad and can present with similar clinical and hematological abnormalities such as anemia, thrombocytopenia, and elevated liver enzymes.
Outcome and follow-up. Complete blood count and peripheral smears were repeated every 24 hours and metabolic markers and electrolytes were closely monitored. Reports for toxoplasmosis, parvovirus, CMV PCR, mononucleosis, and HSV all returned negative. He was discharged on day 5 of admission from the tertiary care hospital, on oral azithromycin (10 mg/kg/dose once daily) and atovaquone (20 mg/kg/dose PO twice daily for 5 more days) with near resolution of anemia (Hgb, 9.9g/dL), improved thrombocytopenia (77 K/uL) continued neutropenia (0.4 K/uL), and a peripheral smear that detected babesia with parasite burden of rounded to 0.0% RBC/HPF.
On day 9 post-discharge, the patient demonstrated full resolution of anemia, thrombocytopenia, hyperbilirubinemia, and transaminitis. Additionally, thick and thin peripheral smear showed no evidence of Babesia. Oral atovaquone and azithromycin were completed after a total of 15 days of therapy. (Figure 2)

Figure 2. Timeline of total patient events since day 1 of illness to full recovery
Discussion. Babesiosis is a tick-borne Zoonotic disease, mostly transmitted by adult ticks and Ixodid scapularis nymph bites, during late spring through summer. symptoms usually occur 1 to 4 weeks after an infected tick bites.1 Transplacental and congenital babesiosis were detected 19 to 41 days after birth, characterized by asymptomatic maternal infection, maternal fever, neonatal fever, anemia, thrombocytopenia. Babesiosis is currently the most common RBC transfusion-transmitted pathogen reported to the FDA. Neonates are more susceptible to numerous infections secondary to immature immune system.
Infection ranges from asymptomatic to potentially fatal disease with severe anemia, thrombocytopenia, hyperbilirubinemia, shock, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and renal failure. Appropriate antimicrobial drug therapy, blood transfusion, and in some cases, and exchange transfusion remain the mainstays of the treatment.6
Babesiosis infection can vary from asymptomatic cases to acute and fatal disease. Asymptomatic and mild infection usually occur in patients who are immunocompetent and have parasitemia less than 4%. Mild to moderate disease symptoms are malaise, fatigue, fever, headache, myalgias, dry cough, nausea and arthralgias. Severe infection presents with nausea, vomiting, high-grade fevers, hemoglobinuria, shock, severe anemia. Risk factors associated with severe disease are parasitemia greater than 4%, neonates, older than 50 years of age, and immunocompromised persons such as with cancer, HIV, hemoglobinopathy, functional asplenia, or chronic heart, lung, or liver diseases.4 Severe complications of babesiosis may include severe anemia, ARDS, DIC, chronic heart failure, myocardial infarction, renal disease, splenic infarcts, or rupture.5 Neonates usually present with fever, anemia, thrombocytopenia, and hepatosplenomegaly. Rash is not usually present. If noted, clinicians should raise suspicion of coinfection with Lyme disease. Fatality rates are 3% to 9%, among hospitalized patients and up to 20% in those patients with immunosuppression.5
Babesiosis is generally diagnosed with microscopy on a blood smear, PCR, and serology. babesiosis is diagnosed by visualization of intra-erythrocytic trophozoites or merozoites on Wright–Giemsa-stained blood smears under oil immersion.6 The level of parasitemia is generally between 1% to 10% but can be as high as 80%. Intracellular Babesia merozoites can be seen in tetrads forming a “Maltese cross” pattern. Laboratory diagnostic features are hemolytic anemia, thrombocytopenia, neutropenia, hyperbilirubinemia, elevated LDH, elevated liver enzymes, elevated BUN, creatinine, and proteinuria. Serology is a useful tool for supporting the diagnosis; however, it may be absent in early disease, and this does not replace microscopy or PCR. A 4–fold rise in Babesia IgG titer helps to differentiate between recent or past infection, which a single positive antibody titer cannot do. IgM and IgG titers > 1:64 are considered positive in most cases. An IgG titer greater than 1:1024 can be detected in acute phase patients and at this level, parasites are visible on blood smears.7 PCR is a more sensitive blood test compared with a blood smear and provides molecular characterization of Babesia species. PCR can be considered of diagnostic benefit when the patient may be early in the phase of infection and parasites may be difficult to visualize on blood smears.8
Per CDC guidelines, the treatment regimen for babesiosis in neonates and infants includes standard 7 to 10 days combination course of clindamycin (5 to 7.5 mg/kg/dose Q 8 hours) and quinine (25 mg/kg/day divided for every 8 hours). Another treatment option includes the combination of azithromycin (12 mg/kg/dose) and atovaquone (40 mg/kg/day divided twice daily) for 7 to 10 days10 or the addition of atovaquone or azithromycin to the clindamycin and quin combination. Exchange transfusion has been recommended by the Infectious Disease Society of America and American Society for Apheresis for patients with high-grade parasitemia greater than 10% or in the presence of significant comorbidities including hemolysis, renal, hepatic, or pulmonary compromise.4 The exchange transfusion has multiple beneficial effects including removal of proinflammatory cytokines and reducing the level of parasitemia.
Conclusion. Emergency room physicians, family physicians, and pediatricians should be mindful of neonatal babesiosis as a potential cause of febrile neonate with evidence of anemia, thrombocytopenia, and hemolysis with hyperbilirubinemia. Prompt history on possible tick bite often yields to early diagnosis and treatment without any delays. Diagnosis of babesiosis should be considered in neonates with conjugated hyperbilirubinemia and elevated liver enzymes of uncertain etiology. PCR blood testing, serological testing, and blood smear examination should be used early in the case of anemia, thrombocytopenia, and neutropenia of a febrile infant. Preterm neonates may need a prolonged course of antibiotics with double volume exchange transfusion to reduce parasite load and for prompt recovery as well.
- About Babesiosis. Centers for Disease Control and Prevention. Available from: Updated, February 12, 2024. Accessed September 27, 2024. https://www.cdc.gov/parasites/Babesiosis/.
- Kjemtrup AM, Conrad PA. Human babesiosis: an emerging tick-borne disease. Int J Parasitol. 2000;30(12,13): 1323-1337. doi:10.1016/s 0020-7519(00)00137-5
- Vannier E, Krause PJ. Human babesiosis. N Engl J Med. 2012;366(25):2397-2407. doi:10.1056/NEJMra1202018.
- Gelfand JA, Vannier EG. Babesiosis: Clinical manifestations and diagnosis. Updated August 2, 2024. Accessed September 27, 2024. https://www.uptodate.com/contents/babesiosis-clinical-manifestations-and-diagnosis.
- Krause PJ, Telford SR 3rd, Ryan R, et al. Diagnosis of babesiosis: evaluation of a serological test for the detection of Babesia microti antibody. J Infectious Dis. 1994;169:923-926. doi:10.1093/infdis/169.4.923.
- Sanchez E, Vannier E, Wormser GP, Hu LT. Diagnosis, treatment and prevention of Lyme disease, human granulocytic anasplasmosis and Babesios review, a review JAMA. 2016;315(16):1767-1777. doi:I:10.1001/jama.2016.2884.
- Recommendations for reducing the risk of transmission transmitted babesiosis, guidance for Industry. US Food and Drug Administration. May 2019. Accessed September 27, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/recommendations-reducing-risk-transfusion-transmitted-babesiosis.
AUTHORS:
Giridhar Guntreddi MD, FAAP, FAPHM1,2 • Alfredo Valdez MD1 • Achuth Jayasankar Kondoor3 • Swayam Prabha Nirujogi MD, MBA, FAAFP4
AFFILIATIONS:
1Sanford Medical Center, Bemidji, MN
2Children’s Hospital of Philadelphia, Philadelphia, PA
3Volunteer student, University of California, Davis, Davis, CA
4Tower Health Medical Group, Reading, PA
CITATION:
Guntreddi G, Valdez A, Kondoor AJ, Nirujogi SP. Neonate with acquired babesiosis. Consultant. Published online October 1, 2024. doi:10.25270/con.2024.10.000001
Received April 3, 2024. Accepted July 19, 2024
DISCLOSURES:
The authors report no relevant financial relationships.
ACKNOWLEDGEMENTS:
None.
CORRESPONDENCE:
Giridhar Guntreddi, MD, FAAP, FAPHM, Sanford Medical Center, 1300 Anne St NW, Bemidji, MN, 56601 (guntreddig@yahoo.com)


